Metacognitive therapy is radically different from other types of psychotherapy because it suggests disengaging from distressing thoughts instead of analyzing, worrying, and controlling them. Many therefore question its validity because it sounds too good to be true: How can doing less to our internal distress help us recover from anxiety and depression?
A recent meta-review showed that MCT effectively treats mental disorders like anxiety and depression and is superior to CBT. In adddition, metacognitive beliefs seem to correlate with vulnerability to psychological disorders, affecting emotional self-regulation negatively.
There is significant scientific evidence supporting the existence of the CAS and metacognitive beliefs in psychological disorders. Here is an overview of the most recent and important studies of Metacognitive therapy.
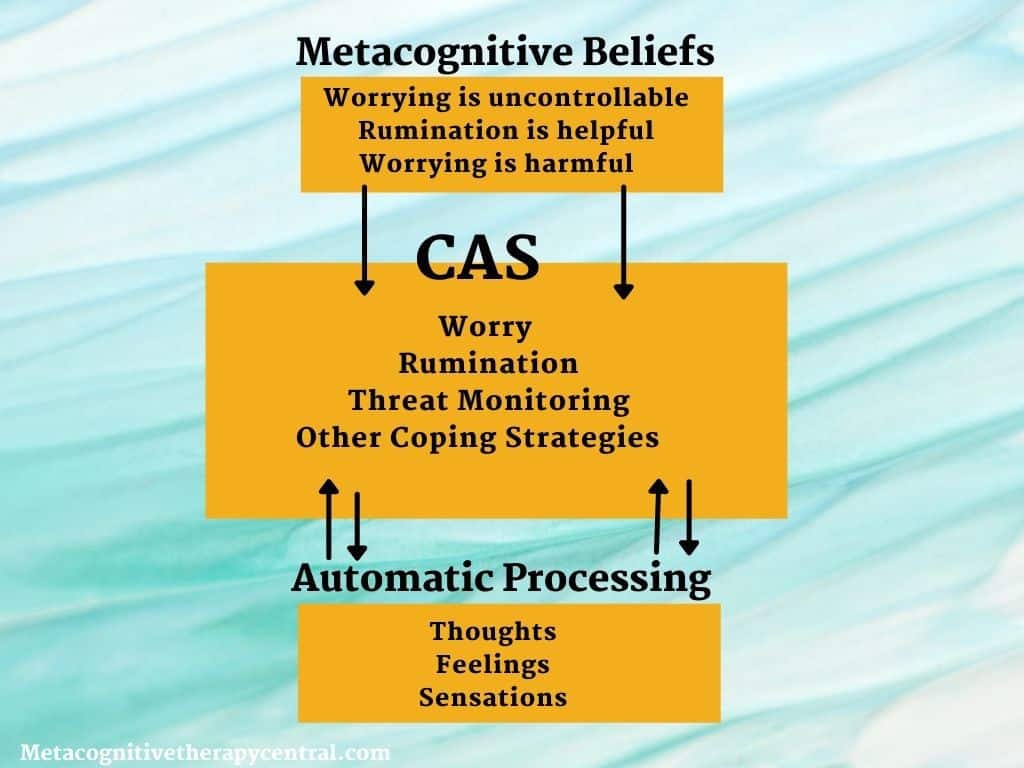
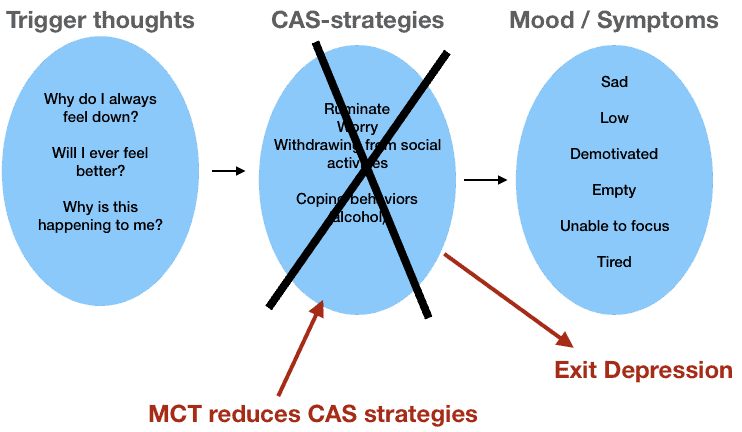
Metacognitive therapy is based on the Self regulatory executive function model (S-REF), stating that the mind can heal itself from distressing thoughts and feelings. According to S-REF, all psychological disorders are caused by the same factors: CAS and metacognitive beliefs. CAS consists of voluntary strategies like rumination and worry. MCT, therefore, focuses on reducing the CAS so that the mind can heal itself from mental illness.
Worry and rumination is bad for emotional well-being
A large database(2) supports how repetitive thinking styles like worry/rumination are unhealthy for emotional well-being.
There is a connection between worry and mental disorders like panic disorder, social phobia, health anxiety, traumatic stress, and generalized anxiety disorder. Similar to worry, rumination is linked to depression (3).
Metacognitive theory suggests that worry has a negative effect on self-regulation, meaning that it blocks emotional processing. Once this natural mechanism is blocked, negative thoughts and feelings persist for a longer time, creating distress for the individual.
Brief periods of worry lead to more anxiety, more depression, less task-focused attention, and more negative thoughts in people who usually worry a lot.
Here are some studies that examined the effects of worry.
| Study | Published | What did they study | What did they find |
| Hazlett-Stevens, Holly & Borkovec, Thomas. Effects of worry and progressive relaxation on the reduction of fear in speech phobia: An investigation of situational exposure. Behavior Therapy – BEHAV THER. 32. 503-517. 10.1016/S0005-7894(01)80033-2. | 2001 | The relationship between worry and speech anxiety (and progressive relaxation) | People who didn’t worry before giving a speech habituated to the anxiety (felt less anxiety over time). However, people who worried did not get used to the situation but continued to feel anxious when giving a speech. Worrying keeps anxiety levels elevated during social performance. |
| Mellings TM, Alden LE. Cognitive processes in social anxiety: the effects of self-focus, rumination and anticipatory processing. Behav Res Ther. 2000 Mar;38(3):243-57. doi: 10.1016/s0005-7967(99)00040-6. PMID: 10665158. | 2000 | How worry, rumination, and self-focus contribute to negative self-judgment after social encounters | When socially anxious people ruminate and worry about their social performance, they risk feeling more anxious and having negative thoughts in their next social interaction. |
| Butler, G., Wells, A., & Dewick, H. Differential effects of worry and imagery after exposure to a stressful stimulus: A pilot study. Behavioural and Cognitive Psychotherapy, 23(1), 45–56. https://doi.org/10.1017/S1352465800017628 | 1995 | How worrying right after a distressing event affects emotional processing | Emotional processing gets blocked by worrying. Participants who worried after watching a scary and stressful movie had significantly more intrusive memories the following 3-days than those who did not worry. |
| Nolen-Hoeksema, S. The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. Journal of Abnormal Psychology, 109(3), 504–511. https://doi.org/10.1037/0021-843X.109.3.504 | 2000 | The role of rumination and depression In a large study of 1,100 adults | Following stressful life experiences, people with clinical depression and a ruminative thinking style had more severe and long-lasting depressive symptoms one year later and less likely to show remission. |
Summary
There is a compelling level of support for worry and rumination contributing to symptoms of emotional disorders like anxiety, depression, and post-traumatic stress.
For more research about worry and anxiety, read this post and this post.
Video: Metacognitive therapy explained
Metacognitive beliefs activate worry and rumination
Metacognitive beliefs mean beliefs about thinking. Metacognitive beliefs are responsible for activating worry and rumination and predict whether someone will develop mental disorders independent of the type of thoughts they think.
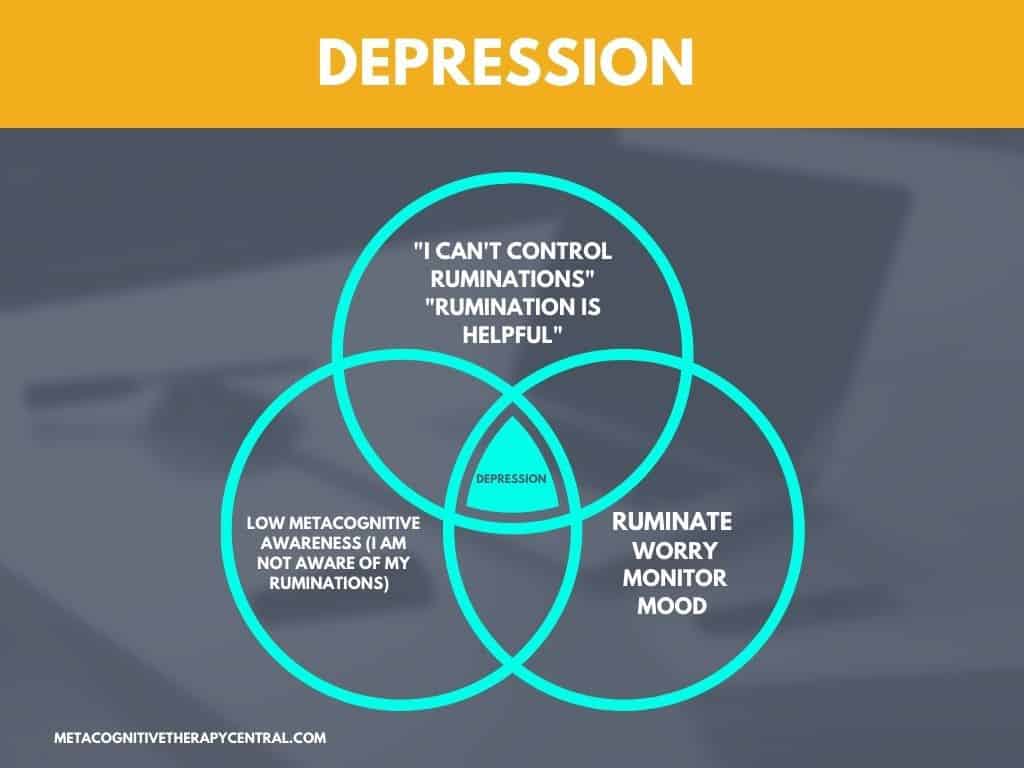
To illustrate the role of metacognitive beliefs, imagine how two students can think the same thought, “I am a failure,” after failing an exam, but only one of them will become depressed. The person who becomes depressed ruminates for days following the exam because he has metacognitive beliefs Ruminating will help me understand (why I am a failure and what I can do about it), and I can’t control my ruminations.
The other student doesn’t have those metacognitive beliefs and might think to himself, “I will study harder and try to do better next time,” and leaves the thought alone.
Here are the most important studies that have examined the effect of metacognitive beliefs on worry and rumination.
| Study | Published | What did they study | What did they find |
| Papageorgiou, C., Wells, A. Metacognitive beliefs about rumination in recurrent major depression, Cognitive and Behavioral Practice, Volume 8, Issue 2, 2001, https://doi.org/10.1016/S1077-7229(01)80021-3. | 2001 | The study interviewed patients with recurrent depression to check for metacognitive beliefs about rumination. | They found out that all depressed patients reported having metacognitive beliefs The study proves that rumination isn’t involuntary, but it is a coping strategy used on purpose because of people’s metacognitive beliefs about rumination. |
| Papageorgiou, C., & Wells, A. Positive Beliefs about Depressive Rumination: Development and Preliminary Validation of a Self-Report Scale. Behavior Therapy. (2001b) 32. 13-26. 10.1016/S0005-7894(01)80041-1. Positive beliefs about depressive rumination: Development and preliminary validation of a self-report scale. Behavior Therapy, Volume 32, Issue 1, (2001c) https://doi.org/10.1016/S0005-7894(01)80041-1. | 2001 | Whether rumination is associated with metacognitive beliefs | Proof that metacognitive beliefs about rumination predict that people become depressed (because they view rumination as helpful). There is a relationship between metacognitive beliefs and developing psychological disorders like anxiety, depression, panic disorder, and social phobia. |
| Wells, A. & Carter, K. Further tests of a cognitive model of generalized anxiety disorder: Metacognitions and worry in GAD, panic disorder, social phobia, depression, and nonpatients, Behavior Therapy, Volume 32, Issue 1, (2001), https://doi.org/10.1016/S0005-7894(01)80045-9. | 2001 | Do patients with generalized anxiety disorder have higher levels of negative metacognitive beliefs? | Patients with generalized anxiety disorder had significantly higher metacognitive beliefs about uncontrollability and the danger of worrying. The paper supports the role of metacognitive beliefs in anxiety disorders |
| Ruscio, A. M., & Borkovec, T. D. Experience and appraisal of worry among high worriers with and without generalized anxiety disorder. Behaviour Research and Therapy, (2004). 42(12), 1469–1482. https://doi.org/10.1016/j.brat.2003.10.007 | 2004 | Why do some people who worry a lot develop generalized anxiety disorder while others don’t? | People with generalized anxiety disorder have more negative metacognitive beliefs about worrying compared to people who also worry a lot. Negative metacognitive beliefs (and not worrying by itself) play an important role in whether someone develops generalized anxiety disorder. |
Summary
There is a lot of scientific support for the role of metacognitive beliefs. Metacognitive beliefs activate the CAS (worry, rumination, and other coping strategies). For example, people who don’t believe in their ability to control worry will start worrying more and use unhelpful coping strategies like alcohol and drugs to control their worrying. In the case of romantic relationships, the CAS consists of starting fights, silent treatments, or avoidance.
Worrying is uncontrollable ( = metacognitive belief about uncontrollability), I could lose my mind with worry ( = metacognitive belief about danger), Worrying could harm my body ( = metacognitive belief about danger), and My thoughts alone have the power to change the course of events ( = thought fusion beliefs seen in people with OCD).
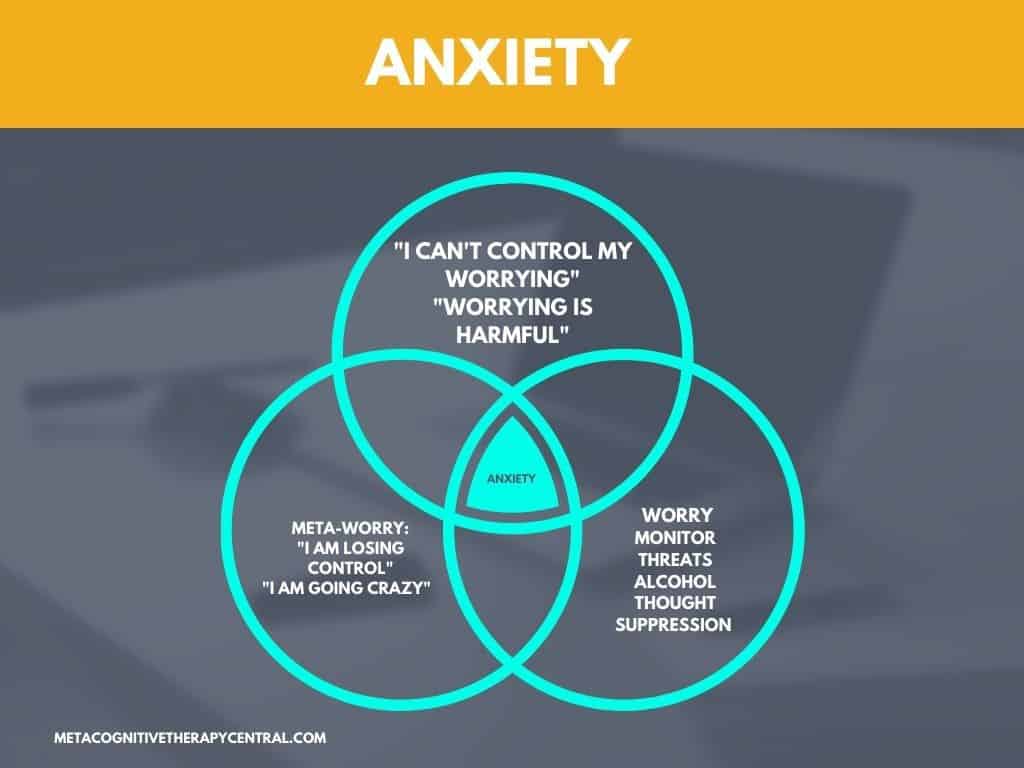
Meta-worry is the negative interpretation of worrying. Examples of meta-worry are: “I am losing control“, “I am going crazy”, “I am harming my body.” Meta-worry increases worry and other unhelpful coping strategies like thought suppression and drinking alcohol.
Metacognitive therapy can treat psychiatric disorders effectively
Obsessive-compulsive disorder
MCT is an effective treatment for OCD (obsessive-compulsive disorder), and it can be offered as a brief therapy. This effectiveness of MCT for OCD is due to the theoretical understanding of OCD:
People develop OCD because
1) the importance people place on their intrusive thoughts
2) the strategies they use to deal with intrusive thoughts
For example, someone has an intrusive thought, “what if I left the stove on?“. The reason that this thought causes so much distress for someone with OCD is that people with OCD have metacognitive beliefs about Thinking certain thoughts make them come true. These metacognitive beliefs are also called thought fusion beliefs (thoughts are fused with reality).
Therefore, someone with OCD is afraid to ignore his intrusive thoughts because he believes his thoughts are 100% true. He might therefore engage in worrying, reassurance seeking, or checking behavior. However, these strategies only provide short-term relief but, in the long term, lead to anxiety and maintain his OCD.
Here are the most important studies that tested the effect of MCT for OCD.
| Study | Published | What did they study? | What did they find? |
| Fisher PL, Wells A. Metacognitive therapy for obsessive-compulsive disorder: a case series. J Behav Ther Exp Psychiatry. 2008 Jun;39(2):117-32. doi: 10.1016/j.jbtep.2006.12.001. Epub 2007 Mar 7. PMID: 17418090. | 2008 | One of the first studies examining the potential of MCT for OCD in four patients | The patients had a 63-75% reduction in OCD symptoms. The patients also reduced their anxiety and depression and improved their metacognitive beliefs about intrusive thoughts. |
| Shareh H, Gharraee B, Atef-Vahid M K, Eftekhar M. Metacognitive Therapy (MCT), Fluvoxamine, and Combined Treatment in Improving Obsessive-Compulsive, Depressive and Anxiety Symptoms in Patients with Obsessive-Compulsive Disorder (OCD). Iran J Psychiatry Behav Sci. 2010;4(2): 17-25. | 2010 | The effectiveness of MCT compared to antidepressant medication for OCD | All the participants who received MCT recovered, compared to 84% of the participants who received both MCT and antidepressant medications. MCT is more effective than antidepressants alone for treating OCD. |
| Van der Heiden, C., Melchior, K., Dekker, A., Damstra, M., Deen, M. Metacognitive therapy for obsessive-compulsive disorder: A pilot study, Journal of Obsessive-Compulsive and Related Disorders, Volume 9, 2016, https://doi.org/10.1016/j.jocrd.2016.02.002. | 2016 | An open trial examining the effectiveness of MCT among 25 patients with OCD | 74% of OCD patients recovered right after treatment, and 80% recovered three months after. The majority of patients 63% and 80%, no longer fulfilled the diagnostic criteria for OCD. |
| Papageorgiou C, Carlile K, Thorgaard S, Waring H, Haslam J, Horne L, Wells A. Group Cognitive-Behavior Therapy or Group Metacognitive Therapy for Obsessive-Compulsive Disorder? Benchmarking and Comparative Effectiveness in a Routine Clinical Service. Front Psychol. 2018 Dec 10;9:2551. doi: 10.3389/fpsyg.2018.02551. | 2018 | Comparing group-delivered MCT with group-delivered CBT for OCD | 86% of patients who received group MCT responded to treatment compared to 64% of those who received group CBT. |
| Glombiewski, J. A., Hansmeier, J., Haberkamp, A., Rief, W., Exner, C. Metacognitive therapy versus exposure and response prevention for obsessive-compulsive disorder – A pilot randomized trial, Journal of Obsessive-Compulsive and Related Disorders, Volume 30, 2021, https://doi.org/10.1016/j.jocrd.2021.100650. | 2021 | Comparing the effectiveness of MCT to ERP (exposure and response prevention) for OCD | Both treatments led to significant improvements. The patients in the MCT group needed less time with the therapist, making MCT equally effective as ERP but less time-consuming. |
Three types of metacognitive beliefs are associated with OCD: thought-event fusion beliefs (thinking something makes it come true), thought-action fusion beliefs (thinking something will make me act on it), and thought-object fusion beliefs (thoughts can be transferred to objects). Because of these beliefs, people with OCD struggle to ignore intrusive thoughts.
Psychosis
Antipsychotic medication is the standard treatment for psychosis. However, many people with psychosis continue to have symptoms and experience cognitive and social difficulties (4).
MCT offers an alternative explanation to how metacognitive beliefs maintain psychotic symptoms because they lead to worry and rumination about hearing voices and having visual hallucinations. According to the research, MCT appears to effectively reduce some psychotic-like symptoms, anxiety, and depression in people at high risk of developing psychosis.
Here is an overview of the research of MCT for psychosis.
| Study | Published | What did they study? | What did they find? |
| Hutton P, Morrison AP, Wardle M, Wells A. Metacognitive therapy in treatment-resistant psychosis: a multiple-baseline study. Behav Cogn Psychother. 2014 Mar;42(2):166-85. doi: 10.1017/S1352465812001026. Epub 2013 Jan 3. PMID: 23286558. | 2014 | Can a short number of MCT sessions reduce delusions, hallucinations, anxiety, and depression in patients with treatment-resistant long-standing psychosis? | Two out of three patients decreased their delusions, depressive symptoms, and anxiety symptoms. One of the patients maintained this effect after three months. |
| Morrison AP, Pyle M, Chapman N, French P, Parker SK, Wells A. Metacognitive therapy in people with a schizophrenia spectrum diagnosis and medication resistant symptoms: a feasibility study. J Behav Ther Exp Psychiatry. 2014 Jun;45(2):280-4. doi: 10.1016/j.jbtep.2013.11.003. Epub 2013 Dec 14. PMID: 24440585. | 2014 | Is MCT feasible for people with psychotic disorders? | The patients had large reductions in their psychotic symptoms and delusions. Reduction in delusions was not maintained after three months. |
| Parker SK, Mulligan LD, Milner P, Bowe S, Palmier-Claus JE. Metacognitive Therapy for Individuals at High Risk of Developing Psychosis: A Pilot Study. Front Psychol. 2020 Jan 17;10:2741. doi: 10.3389/fpsyg.2019.02741. PMID: 32010004; PMCID: PMC6978773. | 2020 | Is MCT a feasible and acceptable treatment for individuals at ultra-high risk of developing psychosis? | 40% of the patients no longer met the “at risk for psychosis” criteria 6 months after treatment. The patients experienced significant improvements in psychotic-like experiences, personal, social, and psychological functioning, and depressive and anxiety symptoms. Negative metacognitive beliefs were also changed. |
Summary
Metacognitive therapy is a promising treatment for obsessive-compulsive disorder. It offers a briefer alternative to treatments like CBT and ERP. MCT is also an acceptable treatment for psychosis. It has been shown to reduce psychotic symptoms, improve anxiety and depression in psychotic (and schizophrenic) patients and lower the risk of developing psychosis in people who are vulnerable. However, to further back up the effect of MCT on psychosis, there is a need for larger studies that include many patients.

Metacognitive therapy is more effective than CBT for depression
Depression is the second largest cause of global disability. It causes great suffering, loss of quality of life, and risk to those who suffer from it. The current effective treatments are antidepressant medications and psychological therapy, mainly CBT, which is the most studied treatment.
Research shows that CBT is as effective as antidepressant medications in the short term but more effective than antidepressant medications over the long term. However, the overall recovery results show that only 50 % of patients who receive CBT clinically recover from depression. Most of these patients also relapse and fall back into depression after treatment (5).
Metacognitive therapy, however, looks very promising for treating depression effectively and preventing relapse. It reduces rumination and worry and changes metacognitive beliefs permanently so that both symptoms and the root cause of depression are effectively dealt with. This is the reason that Metacognitive therapy works better than CBT.
This is the largest study comparing MCT with CBT for depression.
| Study | Published | What did they study? | What did they find? |
| Callesen, P., Reeves, D., Heal, C. et al. Metacognitive Therapy versus Cognitive Behaviour Therapy in Adults with Major Depression: A Parallel Single-Blind Randomised Trial. Sci Rep 10, 7878 (2020). https://doi.org/10.1038/s41598-020-64577-1 | 2020 | The effect of MCT compared to CBT in adults with major depressive disorder. | 74% of patients receiving MCT recovered from depression compared to 52% receiving CBT. After six months, the results were 74% for MCT and 56% for CBT. |
Conclusion
The effectiveness of MCT has been well tested in patients with depression and anxiety disorders. It is also proving to be effective in treating psychiatric disorders like psychosis, OCD, and PTSD, which can potentially elevate MCT´s status as equal to or even better than CBT in the future.
Criticism of Metacognitive therapy
MCT research has some limitations. Firstly, there is a lack of randomized controlled trials to test it’s effectiveness for psychiatric disorders. Secondly, there is a lack of control groups in the available studies, and most of the studies don’t have long term follow up (to measure the effect of MCT after several months or years). This makes it more difficult to draw strong conclusions from the studies. Thirdly, most studies have recruited a very small number of patients, which can make it harder to generalize the effect of MCT.
Another critique of MCT is that most studies have been published by the same group of researchers who developed MCT. This raises the concern that the results of the studies could be biased.
Therefore, to confidently determine the long term effect of MCT, the is a need for
- large trials that tests the effect across different populations
- comparison of MCT to well established treatments like CBT
- MCT’s effect on neurobiology
- MCT’s effect on people who haven’t yet developed metacognitions (like children or people with cognitive disorders)
References
- Photo by Chris Liverani – Unsplash
- Normann N, Morina N. The Efficacy of Metacognitive Therapy: A Systematic Review and Meta-Analysis. Front Psychol. 2018 Nov 14;9:2211. doi: 10.3389/fpsyg.2018.02211. PMID: 30487770; PMCID: PMC6246690.
- Wells, A. (2009). Metacognitive therapy for anxiety and depression. Guilford Press.
- Sharma V, Sagar R, Kaloiya G, Mehta M. The Scope of Metacognitive Therapy in the Treatment of Psychiatric Disorders. Cureus. 2022 Mar 23;14(3):e23424. doi: 10.7759/cureus.23424. PMID: 35475111; PMCID: PMC9030663.
- Johnsen, T. J., & Friborg, O. (2015). The effects of cognitive behavioral therapy as an anti-depressive treatment is falling: A meta-analysis. Psychological Bulletin, 141(4), 747–768. https://doi.org/10.1037/bul0000015
- Photo by Ryan Gagnon – Unsplash