Posttraumatic stress disorder (PTSD) is a chronic mental health disorder linked to traumatic life events. PTSD develops in 1 out of 4 people, and current therapies focus on exposure to traumatic memories. But the effect of these trauma-focused therapies is not high. For example, 60% to 72% of military patients do not improve from PTSD after trauma-focused treatment.
Metacognitive therapy for PTSD can be a quick and effective treatment. It can treat PTSD patients in 10-15 sessions with a recovery rate of 60-85%. Treatment focuses on reducing unhelpful coping like rumination and threat monitoring without the risk of retraumatizing patients.
Metacognitive therapy, MCT, shows better recovery effects for PTSD than recommended therapies like CBT, EMDR, and antidepressants. MCT allows the mind’s self-corrective ability to work, so there is no need to expose PTSD patients to the trauma or use distractions to reduce PTSD symptoms. Therefore, MCT is time-saving and cost-effective, and it is gentle for the patient and the therapist.
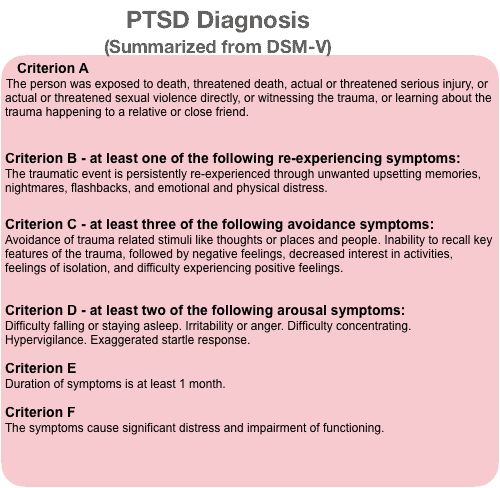
What is Posttraumatic stress disorder (PTSD)?
PTSD symptoms range from anxiety, hypervigilance, irritability, anger, and detachment from feelings. Some people also get intrusive thoughts and memories from the trauma, have nightmares, and have sleep difficulties. People with PTSD go to great lengths to avoid thoughts, feelings, memories, and places linked to the traumatic event.
Metacognitive therapy for PTSD focuses on a self-corrective process
Most people who experience traumatic events recover spontaneously without any help. Even when they experience intense stress and discomfort right after the trauma, 3/4 of people don’t develop PTSD (3) (4).
So how can it be that some people recover on their own and some don’t?
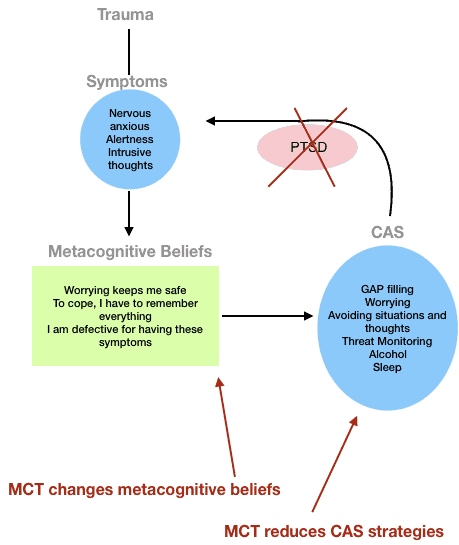
According to Wells and Nordahl (5), the mind has a spontaneous self-corrective process. It is like the body’s ability to heal wounds and broken bones on its own. The mind’s self-corrective process can heal us from negative thoughts and symptoms. Even after highly traumatic events, the self-corrective process prevents PTSD from developing.
For example, someone might feel anxious, shocked, and scared after being in a car accident and get reminders of the car crash from his memory. These feelings, however, will go away on their own after some weeks, and that person can move on with life without constant reminders of the event. This is because of the self-corrective process working. And it happens without therapy.
The self-corrective process is called the Reflexive adaptation process, RAP.
RAP – Reflexive adaptation process
RAP is a natural process that creates a mental plan for survival in people who have survived trauma. In RAP, mental images of the trauma keep entering the mind together with symptoms of anxiety. The purpose of these mental images is for people to imagine dealing with the trauma in different ways. It is a way of preparing for future threats, and it has survival value. The RAP keeps people in a prepared state to deal with danger for days to weeks (3) (5).
RAP is a normal mental process that creates anxiety symptoms and intrusive thoughts (flashbacks) after a traumatic event. When RAP is not dealt with, it stops on its own after a few weeks.
Acute stress is normal after traumatic events
Acute stress and discomfort are part of the RAP and a normal process that everyone goes through after a traumatic event. Acute stress symptoms are usually
- anxiety
- hypervigilance
- distressing thoughts and images from the trauma
Acute stress symptoms go away after four weeks after the traumatic event. The symptoms of anxiety and intrusive thoughts subside so that 3/4 of people recover spontaneously (5).
But since 1 out of 4 people develop PTSD, what interferes with the ability to recover from traumatic events? What hinders the RAP process from helping recovery?

Problematic coping strategies maintain PTSD
People with PTSD engage in problematic coping strategies. To deal with the anxiety from the trauma, they ruminate, worry, and suppress intrusive thoughts. They might also try to avoid situations and people and check their surroundings for danger. Some people start drinking more alcohol to calm their nerves.
These coping strategies are part of the CAS (the Cognitive attentional syndrome), a syndrome that maintains mental problems like anxiety and depression.
The CAS prevents people from recovering from their acute stress symptoms. Coping strategies like rumination and monitoring for dangers prevent the mind’s self-corrective process. Even subtle coping strategies used right after the traumatic event increase the risk of PTSD. According to Wells, subtle coping strategies like going through the event in the mind or talking to a therapist could do more harm than good (5).
So it seems that the more people do to get rid of their symptoms right after a traumatic event, the higher the risk for developing PTSD.
Unhelpful CAS strategies in PTSD
People who have PTSD tend to use one or more of the following CAS strategies (3) (5):
Rumination and analysis. Often, people ruminate about the traumatic event. They ruminate about what they could have done differently and why it happened to them. The purpose of the rumination is to understand what happened and finally be able to move on. However, once they start ruminating, they can’t stop. Their mood gets worse, and their symptoms increase, which leads to more rumination. Hence the vicious cycle continues.
Worry. People with PTSD worry about future dangers because they want to prepare themselves. What if something similar happens again? They also worry about their reactions to the trauma and their symptoms. It is common for them to think that intrusive thoughts make them lose their mind, go crazy, or become psychotic.
Gap filling. Gap filling means trying to get a clear image of what happened at the traumatic event. It is normal not to remember past events in detail. But, PTSD patients think that gaps in their memory is a sign that they are permanently damaged. Therefore they spend hours trying to remember the traumatic event in detail. This is to make sure that they did not leave out any important details.
Monitoring Behavior. To keep themselves prepared for danger, PTSD patients monitor their environment for threats. They also check for specific thoughts, physical symptoms, and intrusions to make sure they don’t lose control or lose their minds.
Avoidance. Certain situations, places, and people can trigger anxiety. People who have PTSD go to great lengths to avoid anything that reminds them of the traumatic event.
Thought suppression. When thoughts and memories from the traumatic event come up, people with PTSD try to push them down. This creates a false sense of being in control but ends up taking all their time and effort.
Maladaptive coping. To feel less anxious and alert, people with PTSD use many different coping strategies. They sleep more, drink alcohol, and watch more tv. Some try not to relax at all because feeling relaxed may trigger PTSD symptoms.
Although some of these strategies are normal to an extent, they hinder the self-corrective process. They prolong PTSD symptoms and make people think they are in danger all the time. This false perception of threat makes people continue to use their unhelpful strategies.
MCT was developed by a British psychologist, Adrian Wells from Manchester University. After 25 years of research into mental illness, Wells discovered that the reason behind mental illness is not grief, accidents, sad feelings, or negative thoughts. It is how we deal with thoughts that create mental illness. When we ruminate, worry, suppress thoughts, or distract ourselves from them, we put ourselves at risk of developing mental disorders. An alternative way to deal with unhelpful thoughts is to observe thoughts and feelings and let them be.
How does Metacognitive therapy treat PTSD?
People with PTSD experience intrusive memories and thoughts from the traumatic event. For some people, their intrusive thoughts feel like being back and re-experiencing the traumatic event. These are called “flashbacks.”
They also experience intense anxiety, nervousness, and feeling on edge. Their brain’s alarm system (the fear network) responsible for detecting danger has become very sensitive. Small indications of danger in the environment can trigger this system, exacerbating PTSD symptoms.
Metacognitive therapy for PTSD helps patients understand that their symptoms are normal and help them reduce their CAS (reducing rumination and worry and focusing attention on neutral things in the environment that doesn’t signal danger). More importantly, Metacognitive therapy helps patients with PTSD to learn that they can control rumination and worry.
Usually, patients with PTSD believe that they can’t stop worrying and that they will go crazy because of worry.
Reducing CAS allows the mind’s self-corrective process to run uninterrupted, leading to recovery from PTSD.
MCT for PTSD: Helps reduce unhelpful coping strategies and make patients aware that they can control what type of thoughts they pay attention to.
Current psychological treatments for PTSD
Common recommendations suggest a trauma-focused approach for PTSD. Trauma-focused treatments go into the memories and talk about the traumatic event. Some treatments try to change unhelpful beliefs about the self, the world, and the future. They also try to create a different and more positive memory of the trauma. The purpose of these therapies is to reduce PTSD symptoms. The assumption is that patients should revisit the trauma in their memories to recover from PTSD (7).
Cognitive Behavioral Therapy, CBT
One of recommended and evidence-based therapies is Cognitive Behavioral Therapy, CBT. CBT treatment includes exposing people to memories of the trauma. This is done by imagining the traumatic event and writing or reading the traumatic memory out loud in detail. This process is called imaginal exposure.
The point is to reduce the patient’s avoidance of trauma reminders and distressing thoughts and reduce anxiety. At the same, it is supposed to move the trauma memories from short-term into long-term memory. Once the memories move to long-term memory, people can remember the important facts of their traumatic experience without reliving most of the pain.
Other Recommended Treatments for PTSD
Other recommended treatments for PTSD are Prolonged Exposure, PE, Trauma-focused CBT, Tf-CBT, and eye movement desensitization therapy, EMDR. Each of these treatments has a large evidence base showing their effectiveness.
Medication Treatments for PTSD
Several medications for the treatment of PTSD are recommended. Among the popular choices are antidepressant medications like Sertraline, Paroxetine, Fluoxetine, and Venlafaxine.
Who makes treatment guidelines for PTSD?
- American Psychological Association
- American Psychiatric Association
- Veterans Health Administration and Department of Defence
- National Institute for Health and Clinical Excellence
- Institute of Medicine

Are trauma-focused therapies effective?
These treatment recommendations have created controversy among treatment providers. Psychologists are concerned that trauma-focused treatments risk re-traumatizing patients. This risk is especially high when treatment focuses on going over the memory of the traumatic event.
Also, exposing patients to traumatic events to recover from PTSD is not scientifically supported.
Most patients tend to drop out of treatment because they want to avoid the discomfort that exposure to the trauma brings. These patients risk developing chronic PTSD that is left untreated for decades.
There is also concern that trauma-focused treatments are ineffective among military people with PTSD. Studies show that 60% to 72% of military patients do not improve from PTSD after trauma-focused treatment.
The results are very problematic because PTSD is so debilitating in all life areas (work, social, and physical problems). It is essential to develop new treatment approaches for PTSD that are both effective and live up to the general requirements for effective psychological treatment.
Metacognitive therapy might be the solution. It is proven effective for PTSD (10). It is already established as a suitable and even better treatment than CBT for mental disorders like anxiety, depression, OCD, and bipolar II disorder.
By letting thoughts and feelings be, the reflexive adaptation process, RAP, is left uninterrupted. The reflexive adaptation process is part of the mind’s self-corrective ability. It helps us to recover from traumatic events. Because of this, Metacognitive therapy looks very promising and helpful for treating PTSD. MCT has proven to reduce PTSD symptoms in 80 percent of patients and prevent relapse (11).
According to American Psychiatric Association (APA), a suitable PTSD treatment should take into account (9):
- A lot of scientific evidence for the treatment
- The benefits of treatment way more than harm or burden to the patient with PTSD
- The patient’s personal values and preferences for the treatment
- The treatment works for different populations (children, adolescents, adults, and the elderly)
Summary
- Metacognitive therapy focuses explicitly on reducing each CAS strategy and noting how much time patients spend ruminating, worrying, and coping.
- The CAS hinders the self-regulating process and keeps the trauma going. Therefore, the work of uncovering all the CAS strategies in detail is crucial in therapy. With a trained MCT therapist, all these strategies will be targeted and reduced successfully.
- Metacognitive therapy is very gentle to both patients and the therapist. The main reason is that MCT therapists don’t address the content of the thoughts or the trauma.
Research on Metacognitive Therapy for PTSD
This article explains treating people with PTSD through Metacognitive therapy techniques. It also explains how metacognitive beliefs (beliefs about thoughts and feelings) potentiate PTSD symptoms. https://www.frontiersin.org/articles/10.3389/fpsyg.2018.01898/full
This study shows that MCT as a non-trauma-focused treatment approach is superior to established trauma-focused treatments. https://www.frontiersin.org/articles/10.3389/fpsyg.2019.00264/full#B29
This article investigates MCT for younger people. It shows that Metacognitive therapy is a feasible and promising treatment for traumatized children and adolescents. https://www.frontiersin.org/articles/10.3389/fpsyg.2019.00264/full
This article explains that coping strategies to reduce symptoms are maladaptive in that they increase and maintain a sense of threat and block emotional processing. https://link.springer.com/article/10.1007/s10608-014-9636-6
This e-book contains a complete overview of scientific articles about Metacognitive therapy. https://www.frontiersin.org/research-topics/7547/metacognitive-therapy-science-and-practice-of-a-paradigm
Where can I get Metacognitive therapy for PTSD?
If you are suffering from PTSD and would like to receive Metacognitive therapy, it is important to find an MCT-I licensed therapist.
AT the MCT-Institue you will find a list of experienced MCT-I licensed therapists that treat a broad range of mental disorders, including PTSD.
References
- Photo by Susan Wilkinson – Unsplash
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
- Wells, A. (2009). Metacognitive therapy for anxiety and depression. Guilford Press.
- Wells A, Colbear JS. Treating posttraumatic stress disorder with metacognitive therapy: a preliminary controlled trial. J Clin Psychol. 2012 Apr;68(4):373-81. doi: 10.1002/jclp.20871. PMID: 24469928.
- Wells A., Nordahl H. Personal communication, Copenhagen (2021)
- Photo by Julia Taubitz – Unsplash
- National Institute for Health and Care Excellence (2018) https://www.nice.org.uk/guidance/ng116/chapter/Recommendations
- Photo by Brett Jordan – Unsplash
- https://www.apa.org/ptsd-guideline
- Sharma V, Sagar R, Kaloiya G, Mehta M. The Scope of Metacognitive Therapy in the Treatment of Psychiatric Disorders. Cureus. 2022 Mar 23;14(3):e23424. doi: 10.7759/cureus.23424. PMID: 35475111; PMCID: PMC9030663.
- Simons M and Kursawe A-L (2019) Metacognitive Therapy for Posttraumatic Stress Disorder in Youth: A Feasibility Study. Front. Psychol. 10:264. doi: 10.3389/fpsyg.2019.00264