Health anxiety (HA) causes great suffering and high health care use (1) (2). Unfortunately, fewer than 50% recover from HA through Cognitive-behavioral therapy (CBT), and this effect declines over time, calling for better treatments (3)(4).
The metacognitive model proves that health anxiety is due to difficulty stopping worrying about symptoms. Health anxiety is therefore not caused by beliefs about being seriously ill, which is the general assumption among mental health professionals.
So instead of reality testing misinterpretations of symptoms, Metacognitive therapy (MCT) for HA helps patients reduce their worries about symptoms and teaches them that they themselves are in control of stopping worry (5).
Would you still worry so much if you learned that your problem is not that you are physically ill but because you think that you are physically ill?
And would your symptoms still be a problem for you if you could stop worrying about them?
Metacognitive therapy for health anxiety: Health anxiety is maintained because you continue to worry about your health.
How does MCT treat health anxiety?
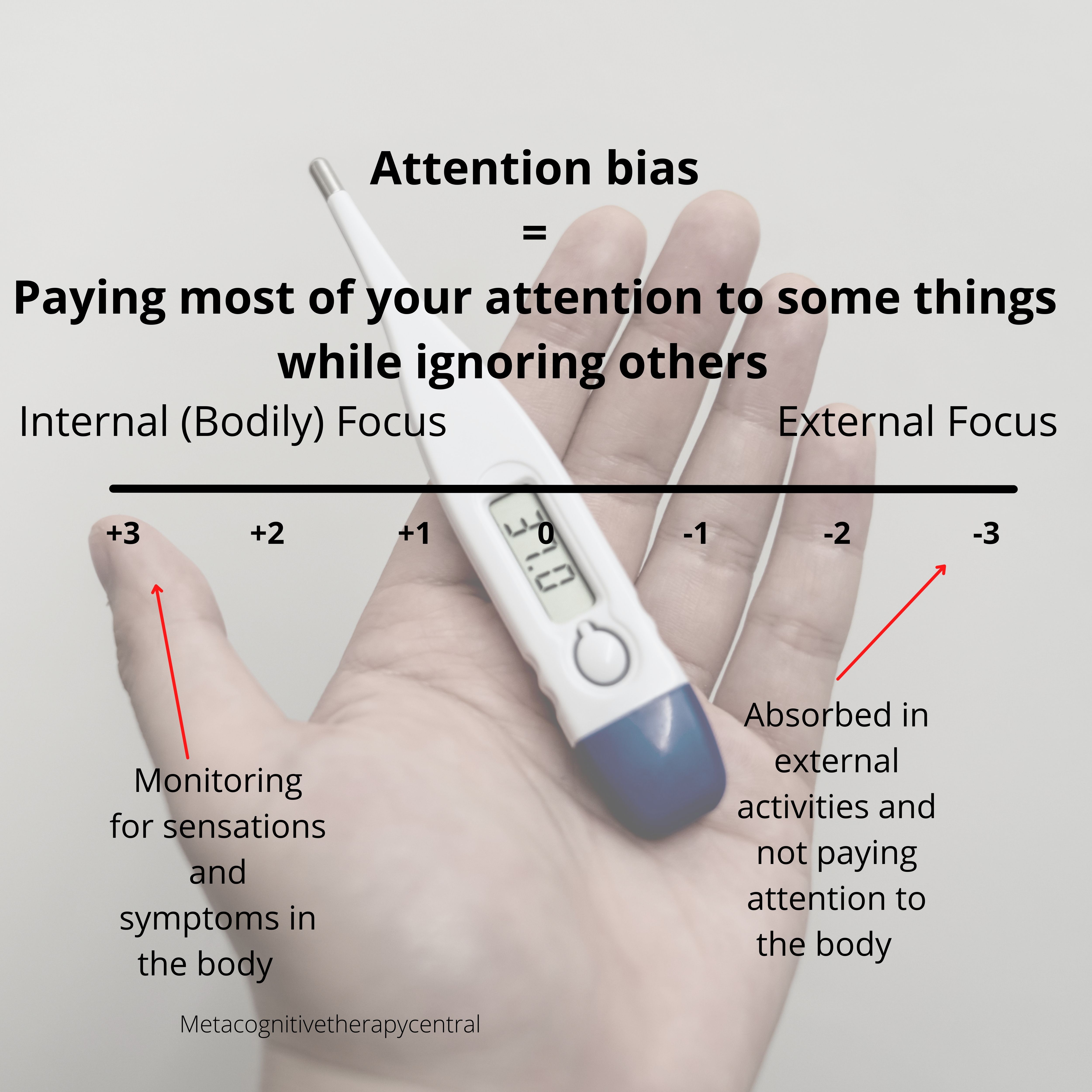
Since people with HA pay a lot of attention to their bodies (a defective strategy called threat monitoring) and worry about bodily sensations, they learn through MCT to interrupt worry with detached mindfulness and shift their focus through attention training techniques (6).
Detached mindfulness and attention training technique provide an alternative to worrying, and they also teach how HA patients have choice and flexibility when responding to anxious thoughts and symptoms.
For example, people with HA typically worry about anxious thoughts like “There is something seriously wrong with me” or “What if the doctor oversaw signs of a serious illness in my body?”
Aside from worrying and threat monitoring, people with HA use the following strategies to cope:
- Rumination
- Body checking
- Seeking reassurance (from searching google to asking family and friends)
- Seeking medical care
- Avoiding situations that cause physical symptoms (for example, specific foods and exercising)
- Trying to control thoughts about illness
However, these strategies are counter-productive and cause more physical and anxiety symptoms.
MCT, therefore, focuses on mapping out each strategy and eliminating it. For treatment to be successful, HA patients need to understand that their coping strategies are the problem and not that they are suffering from an undiscovered serious illness. This is called creating a Metacognitive case formulation (see illustration below).
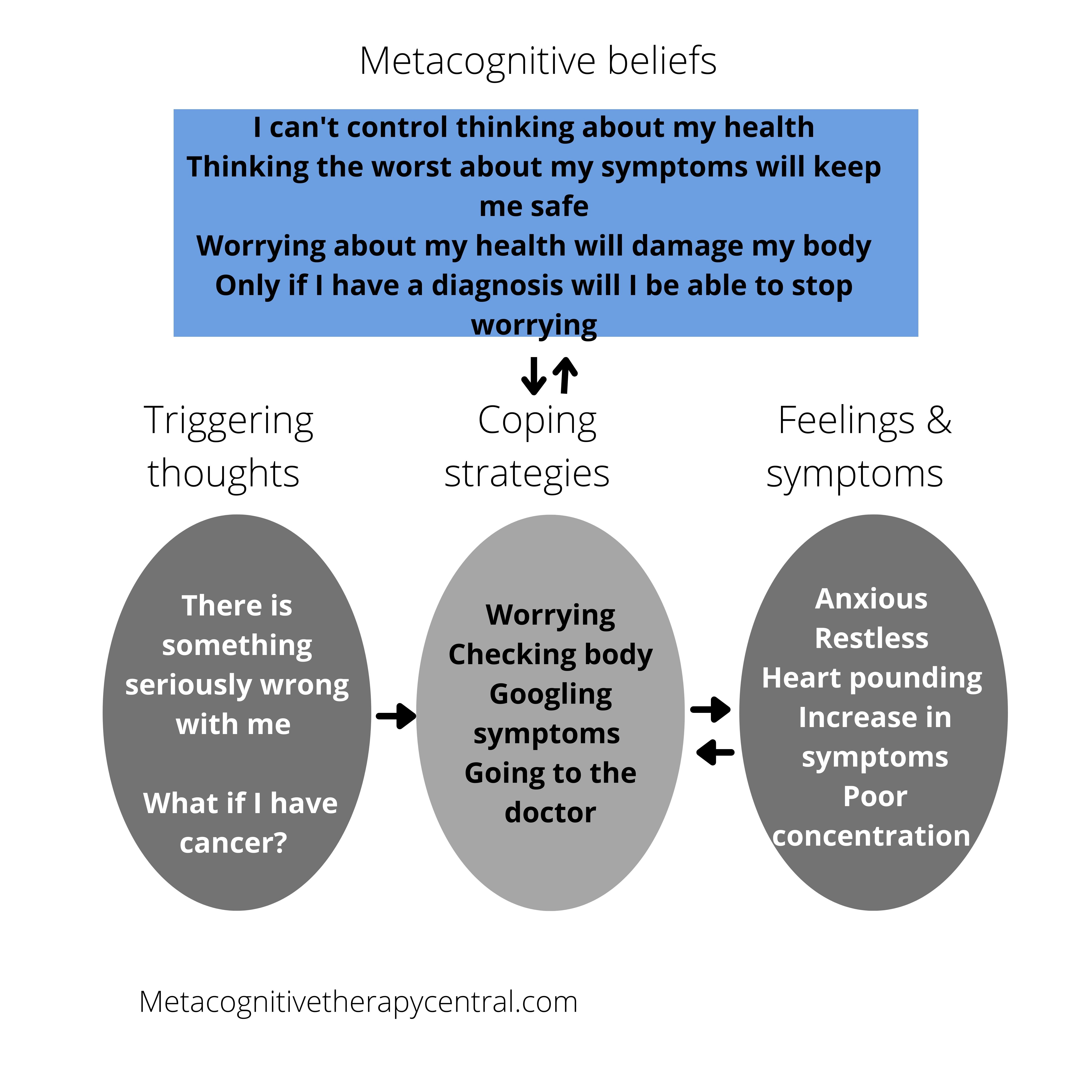
According to Bailey and Wells (7), the metacognitive model of HA shows that people with HA start worrying when they notice physical sensations because of their positive metacognitive beliefs: Thinking the worst about my symptoms will keep me safe.
At the same time, negative metacognitive beliefs make people with HA believe that they can’t control their worrying. They believe that once they start worrying, “What if something is wrong, what if I am really ill, how will I cope? What about my children? Should I call the doctor again? This is too much; I need to know now….” they won’t be able to stop.
The model also shows that worrying only exacerbates physical symptoms like pains, aches, and physical arousal, leading to more negative thoughts about illness.
- Worry, rumination, threat monitoring, and reassurance seeking exacerbate health anxiety symptoms
- Worry, rumination, threat monitoring, and reassurance seeking are part of the cognitive attentional syndrome, CAS
- CAS is controlled by metacognitive beliefs that are beliefs about thinking
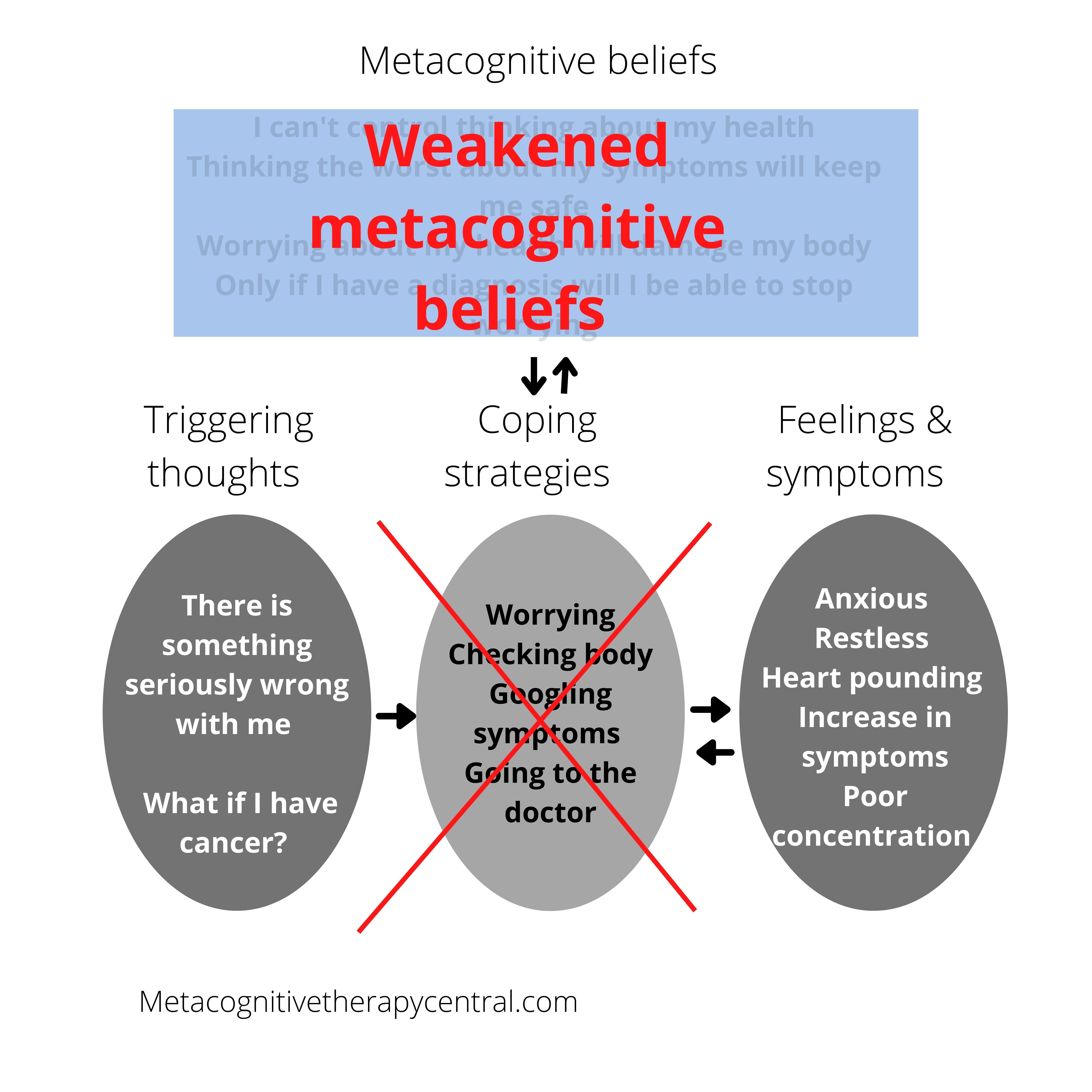
MCT will remove the CAS through metacognitive beliefs
MCT for HA will therefore remove all CAS strategies by teaching the patient that worrying is not helpful and that it can be controlled.
One way to challenge the belief that worrying is unhelpful is to make the patient worry more to see whether more signs of illnesses will be detected and prevented. If worrying about illness is really helpful, the patient will discover more illnesses. However, patients with HA find out that worrying does not lead to feeling more ready or detecting more signs of danger, but that worrying only intensifies their anxiety.
Challenging the patient’s logic is very effective in changing their metacognitive beliefs. And once their metacognitive beliefs are changed, they will no longer worry or use any CAS strategies. This, in turn, allows for healthy emotion processing (also called self-regulation) and recovery from HA in the long term.
Examples of metacognitive beliefs in health anxiety
Positive metacognitive beliefs in HA hold information about worrying about illness is useful. So despite being in a positive state of mind, people with HA still believe that worrying is a good thing, for example, to prevent them from becoming ill.
Examples of positive metacognitive beliefs in HA:
“thinking the worst about symptoms will keep me safe”
“thinking positively about my health will tempt fate, and I will become ill”
Negative metacognitive beliefs in HA are about the uncontrollability of illness-related thinking. For example, people with HA don’t believe in their ability to control worry on their own and need help from doctors and from seeking reassurance from others. Besides, not believing that they can stop worrying prevents them from doing so. So instead, they try to stop worrying through strategies like thought control and reassurance seeking, which backfire in the end (5).
Examples of negative metacognitive beliefs:
“I have no control over thinking about my health”
“Only if I have a diagnosis will I be able to stop worrying”
“worrying about my health will damage my body”
MCT will help to refocus attention
The work of Wells has earlier shown that teaching HA patients to move their attention away from being constantly focused on their bodies and out on neutral things helps tremendously with recovery.
Patients with HA have selective attention that is biased toward bodily sensations. This means that they have taught themselves to pay more attention to their bodies and therefore discover more natural symptom fluctuations in the body that most people ignore.

In therapy, HA patients learn that they can pay attention to other things than their bodies and worry less about normal body fluctuations. For example, they learn that by increasing attention paid to symptoms on purpose, those symptoms intensify, and that biased attention doesn’t provide accurate information about sickness.
- Metacognitive beliefs make people with health anxiety use unhelpful coping strategies like worry and reassurance seeking
- Metacognitive beliefs increase the belief that worrying can’t be stopped
- Excessive attention on body sensations intensifies these sensations
- Biased attention on the body is not a reliable way to detect serious illness
MCT vs. CBT for treating health anxiety
CBT
A systematic review of all the studies on CBT for HA shows that recovery rates from HA are between 30 and 50% (3).
Besides, in a recent study (4) on the effectiveness of CBT for HA, it seems that the effect of CBT for HA dramatically drops after treatment ends.
This study (8) found that other (non-specific treatments) that were not intended to treat HA provided the same results as CBT treatments after 12 months.
A study by Bailey and Wells (9) suggests that the dropping effect of CBT is because CBT only targets maintenance factors (stopping negative thoughts about illness) but doesn’t deal with important factors like metacognitive beliefs. On top of that, the CBT research doesn’t clearly describe which specific CBT elements are responsible for treatment effects. This makes it hard to determine which elements of CBT cause improvement for patients with HA.
For a quick overview of the differences between MCT and CBT, read this post.
MCT
Papageorgiou and Wells (6) found that attention training created big changes in three patients suffering from HA, causing a reduction in health-related worrying, threat monitoring, and beliefs about illness. The effect was maintained after six months.
This study (10) also used attention training on HA patients and found that it reduced attention to bodily sensations and health-related anxieties.
Based on the research, it looks like MCT is a promising therapy for HA. This is because metacognitive beliefs better predict whether someone develops HA than thoughts about illness (11). Metacognitive beliefs also better predict when someone gets HA compared to theories about misinterpretations of anxiety symptoms (12).
- Cognitive-behavioral therapies (CBT) help 30-50% with recovery from health anxiety
- The effect of CBT drops after treatment
- Metacognitive therapy (MCT) is a promising treatment for health anxiety
Summary
Instead of focusing on changing the thoughts about illness, therapy for HA should focus on changing metacognitive beliefs. Changing metacognitive beliefs and bringing worrying under control is the core intervention in MCT, which will help HA patients recover faster and maintain the effect.
Is health anxiety OCD?
Health anxiety is not OCD. Health anxiety is mainly driven by uncontrollability metacognitive beliefs, similar to generalized anxiety disorder. In contrast, OCD is driven by fusion metacognitive beliefs making people believe in the reality of intrusive thoughts.
Although some people with health anxiety strongly believe that thoughts can cause illness, MCT therapists follow a manual for generalized anxiety disorder to treat health anxiety and not an OCD manual.
Does reducing worry lead to overlooking a severe illness?
Reducing worry will help HA patients discover that worry fuelled their HA and not because they suffer from a serious illness. They also learn that they can reduce worrying and, at the same time, take good care of their health, for example, by designating specific times to visit the GP and do routine health checks.
Sources
- Lucock & Morley, 1996; Noyes, et al., 1993; Robbins & Kirmayer, 1996; Sunderland, Newby, & Andrews, 2013)
- Lee S, Creed FH, Ma YL, Leung CM. Somatic symptom burden and health anxiety in the population and their correlates. J Psychosom Res. 2015 Jan;78(1):71-6. doi: 10.1016/j.jpsychores.2014.11.012. Epub 2014 Nov 15. PMID: 25466323.
- Olde Hartman TC, Borghuis MS, Lucassen PL, van de Laar FA, Speckens AE, van Weel C. Medically unexplained symptoms, somatisation disorder and hypochondriasis: course and prognosis. A systematic review. J Psychosom Res. 2009 May;66(5):363-77. doi: 10.1016/j.jpsychores.2008.09.018. Epub 2008 Dec 16. PMID: 19379952.
- Olatunji BO, Kauffman BY, Meltzer S, Davis ML, Smits JA, Powers MB. Cognitive-behavioral therapy for hypochondriasis/health anxiety: a meta-analysis of treatment outcome and moderators. Behav Res Ther. 2014 Jul;58:65-74. doi: 10.1016/j.brat.2014.05.002. Epub 2014 May 24. PMID: 24954212.
- Wells, A. (2009). Metacognitive therapy for anxiety and depression. Guilford Press.
- Papageorgiou, C., & Wells, A. (1998). Effects of attention training on hypochondriasis: A brief case series. Psychological Medicine, 28(1), 193–200. https://doi.org/10.1017/S0033291797005825
- Bailey R, Wells A. Development and initial validation of a measure of metacognitive beliefs in health anxiety: The MCQ-HA. Psychiatry Res. 2015 Dec 30;230(3):871-7. doi: 10.1016/j.psychres.2015.11.035. Epub 2015 Nov 25. PMID: 26626951.
- Clark DM, Salkovskis PM, Hackmann A, Wells A, Fennell M, Ludgate J, Ahmad S, Richards HC, Gelder M. Two psychological treatments for hypochondriasis. A randomised controlled trial. Br J Psychiatry. 1998 Sep;173:218-25. doi: 10.1192/bjp.173.3.218. PMID: 9926097.
- Bailey, R & Wells, A 2013, ‘Does metacognition make a unique contribution to health anxiety when controlling for neuroticism, illness cognition, and somatosensory amplification?‘, Journal of Cognitive Psychotherapy, vol. 27, no. 4. https://doi.org/10.1891/0889-8391.27.4.327
- Weck, Florian & Neng, Julia & Richtberg, Samantha & Jakob, Marion & Stangier, Ulrich. (2014). Cognitive Therapy Versus Exposure Therapy for Hypochondriasis (Health Anxiety): A Randomized Controlled Trial. Journal of consulting and clinical psychology. 83. 10.1037/ccp0000013.
- Bailey, R., & Wells, A. (2016). The contribution of metacognitive beliefs and dysfunctional illness beliefs in predicting health anxiety: An evaluation of the metacognitive versus the cognitive models. Clinical Psychologist, 20(3), 129–137. https://doi.org/10.1111/cp.12078
- Bailey, Robin & Wells, Adrian. (2015). Metacognitive Beliefs Moderate the Relationship between Catastrophic Misinterpretation and Health Anxiety. Journal of Anxiety Disorders. 34. 10.1016/j.janxdis.2015.05.005.
- Photo by Winel Sutanto – Unsplash