
What is the difference between those who develop anxiety and depression and those who don’t?
Imagine dealing with negative thoughts in a totally different way that seriously boosts your mental health. This approach could keep you from getting stuck in anxiety, depression, or OCD. On top of that, you would also feel better, focus sharper, and build mental strength. That is exactly what you learn in Metacognitive therapy.
Metacognitive Therapy (MCT) is grounded in a proven theory: the mind can self-heal from distressing thoughts and experiences, provided we stop ruminating and worrying about them. The therapy reduces these unhelpful thinking patterns and promotes a healthier relationship with negative thoughts.
MCT was developed by Professor Adrian Wells at the University of Manchester, UK. According to Professor Wells, thinking styles like worry and rumination can interfere with recovery from mental illness, and therefore, reducing them is the primary goal of MCT (1).




“Everyone has negative thoughts and everyone believes their negative thoughts sometimes. But not everyone develops sustained anxiety, depression, or emotional suffering.”
Adrian Wells, PhD, Clinical Psychologist and founder of MCT
What is Metacognitive therapy?
Metacognitive therapy, MCT, is a psychotherapy that helps people reduce dysfunctional thinking styles like rumination and worry, and challenge and change metacognitive beliefs that are thought to contribute to these processes.
After 25 years of research into mental illness, Wells discovered that a factor beneath mental illness is not grief, accidents, sad feelings, or negative thoughts but how we deal with thoughts.
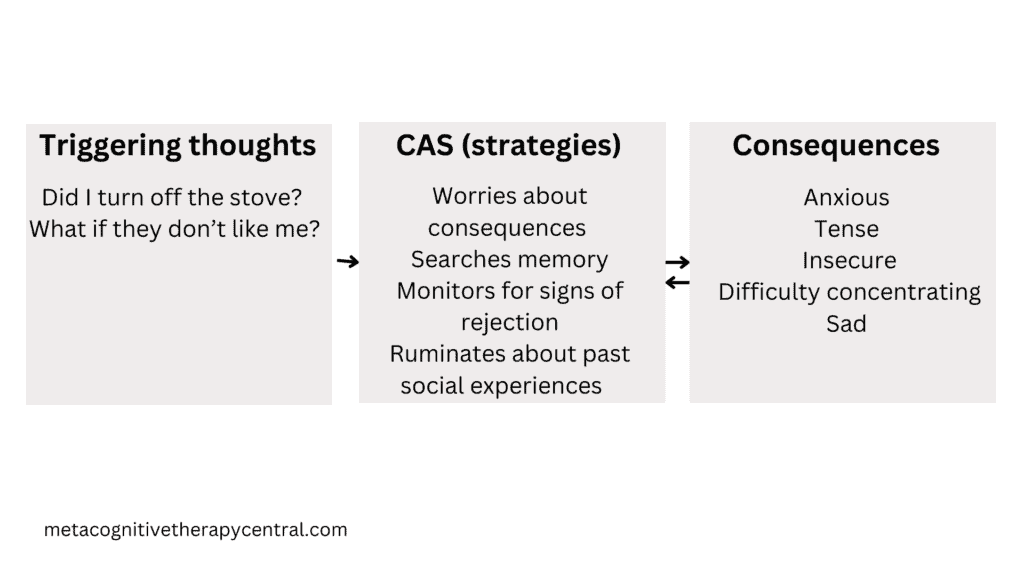
When we ruminate, worry, suppress thoughts, or distract ourselves from them, we put ourselves at risk of developing greater psychological symptoms. Wells and Matthews (1994) identified a pattern of responses to negative thoughts that they called the Cognitive Attentional Syndrome (CAS) (2).
CAS is controlled by biased metacognition, which includes knowledge about thoughts. This is why the therapy developed is called Meta-cognitive therapy.
Reducing CAS requires working on several levels of the metacognitive system and this will take a skilled MCT therapist about 10 sessions. One of the ways this is achieved is through a strategy called detached mindfulness.
| What is it? | MCT is a psychotherapy (talk therapy) based on information processing theory. |
| How does it view mental illness? | Mental illness is maintained through prolonged thinking styles like rumination and worry. These thinking styles prevent the mind from regulating emotions on its own and thereby prolong emotional suffering |
| What can it do? | MCT treats mental disorders like anxiety, depression, OCD, social phobia, PTSD, and borderline personality disorder |
| How does it work? | MCT works by reducing unhelpful thinking patterns like rumination, worry, and threat monitoring. It also changes metacognitive beliefs that are responsible for activating these unhelpful thinking styles |
| How effective is it? | MCT has a 74-80% success rate for treating depression and anxiety disorders (compared to 54% in cognitive behavioral therapy) |
| How many sessions is required? | 10 sessions |
| What is required of clients? | The client should be willing to actively participate in treatment through in-session experiments and by applying new MCT strategies for homework |
| What does MCT not include? | MCT does not include meditation, applied relaxation, breathing techniques, or cognitive restructuring |
| MCT in a nutshell | Thoughts are brief and harmless. Worrying and ruminating about them will make you feel worse. You can learn to stop worry and rumination. |
How does MCT work?
To understand how MCT works, it is important to look at the interactions that happen in the human brain. Adrian Wells, the founder of Metacognitive Therapy (MCT), introduced a significant theory in 2019 about how MCT influences the brain(10). This theory, known as the Metacognitive Control System (MCS), proposes that our brain has two main thinking systems: the MCS, which holds our metacognitive knowledge, and the CS (Cognitive System), where our actual thinking processes take place.
The Metacognitive Control System (MCS) is like the brain’s supervisor, keeping an eye on how we think. It decides things like whether we get stuck ruminating about problems in our Cognitive System (CS). Plus, it affects our brain wiring, influencing gut feelings, control over impulses, and how alert we are.
On the other hand, the CS is where the action happens—the place for all our active thinking, whether it’s worrying, daydreaming, or trying hard to push thoughts away.
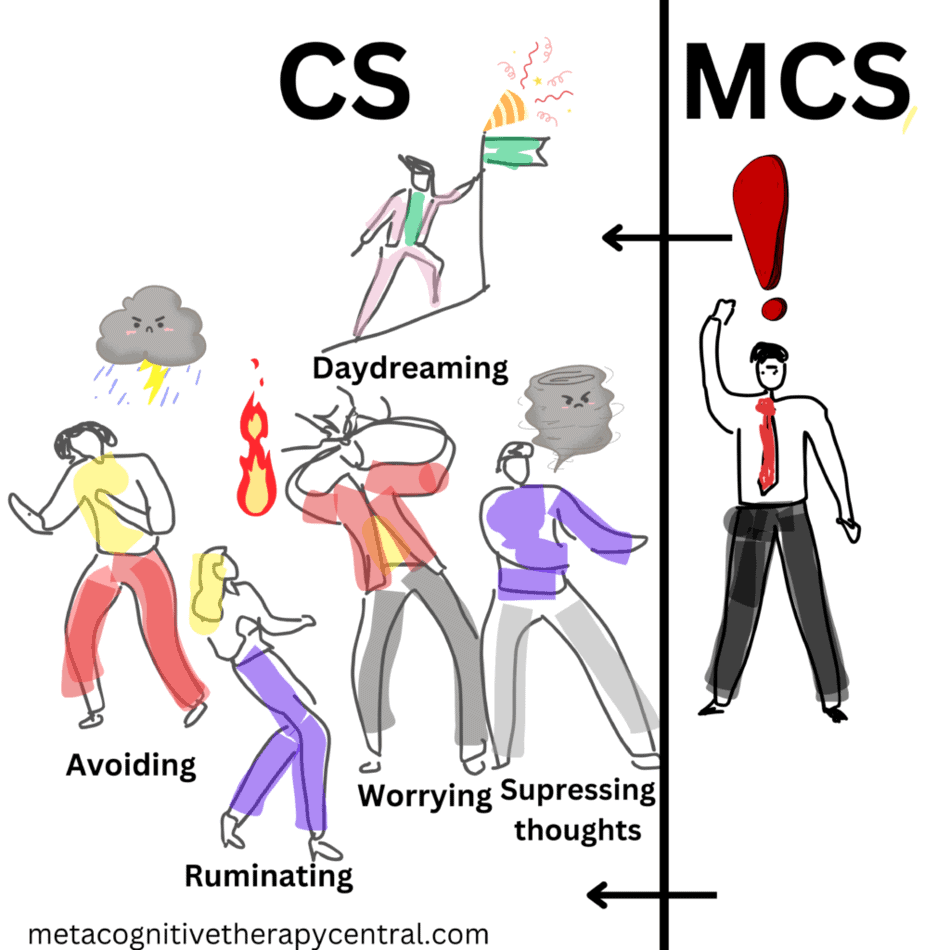
Understanding how these two systems interact is key. The MCS essentially watches and directs what is going on in the CS. It follows a kind of “how-to-think” guide, which is also known as metacognitive information or metacognitive beliefs.
For example, if someone’s “how-to-think” guide says, “I need to worry a lot to solve my problems,” they might start worrying when a negative thought comes up (like being anxious about whether they turned off the stove).
This separation of brain systems by Wells isn’t just an interesting fact but it is very important for understanding mental illness and figuring out how to treat them effectively.
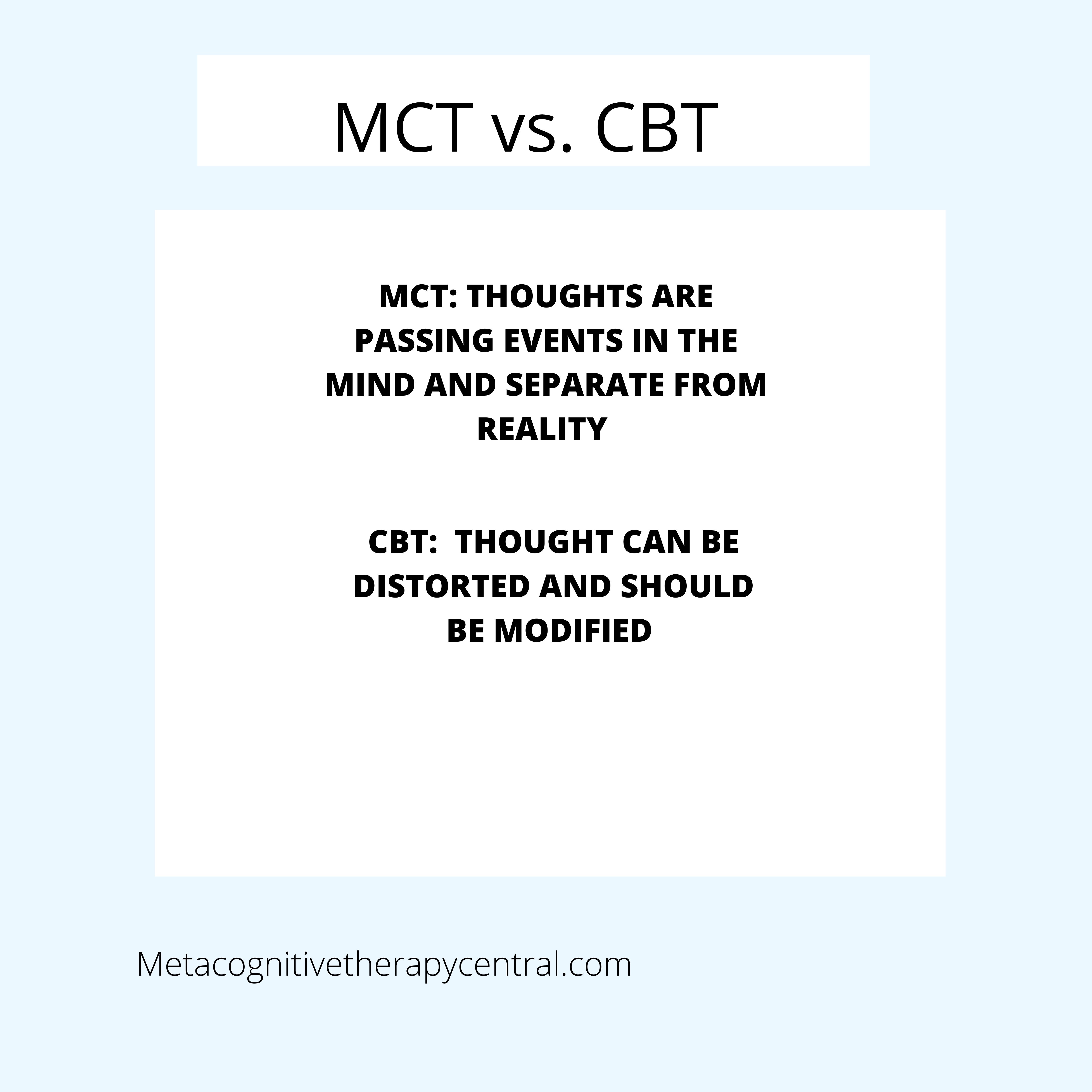
Wells argues that to recover from mental health issues, we should tweak this “how-to-think” guide in the MCS rather than just playing around with what’s going on in the CS (like changing negative thoughts to more realistic ones, as often done in cognitive-behavioral therapy).
By adjusting this “how-to-think” guide in the MCS, we can reduce overthinking and worrying and cut down the risk of falling into mental disorders. That is why Metacognitive Therapy is so different than any other known psychotherapy: it focuses on thinking about thinking because that is more important helping people recover from mental illness.

What is the CAS?
CAS stands for the Cognitive Attentional Syndrome and consists of unhelpful coping strategies that take place in the CS. There are four main categories:
1) Rumination
2) Worry
3) Threat monitoring (looking for bodily symptoms and potential dangers)
4) Other unhelpful coping behaviors (avoiding situations, too much sleep/rest, alcohol, binge eating, procrastinating, etc.)
People with mental illnesses use one or more of these strategies in excess. They ruminate for many hours every day, worry, and check their mood. Often, they also try to numb their thoughts with alcohol, sweets, or distractions.
These strategies are used with good intentions. People ruminate to solve their problems and feel better. Or they worry to be prepared. Unfortunately, they will experience the opposite effect because the CAS backfires, and leave people more depressed, anxious, stressed, and confused.
What are metacognitive beliefs?
Metacognition means thinking about thinking. Metacognitive beliefs are beliefs that shape what we pay attention to internally. Metacognitive beliefs also decide what strategies we use to handle thoughts and feelings.
There are two types of metacognitive beliefs, positive and negative.
Positive metacognitive beliefs tell us to think more about negative thoughts and feelings because doing that is helpful.
Examples of positive metacognitive beliefs are
Worrying will help me cope
Rumination will help me understand
Negative metacognitive beliefs tell us that specific thoughts and feelings are harmful and that we can’t control worry and rumination.
Examples of negative metacognitive beliefs are
My worrying is uncontrollable
I cannot stop ruminating
Worrying is harmful
It is common to hold a mix of positive and negative metacognitive beliefs. However, according to Wells, negative metacognitive beliefs play a significant role in predisposing someone to mental disorders like anxiety (4).
When we hold negative metacognitive beliefs like “I can’t stop overthinking, I’m losing it,” we feel stuck in a loop of rumination and worry. We think we have no choice but to keep going, sometimes for hours or even days. And because overthinking keeps us feeling down, we’re tempted to use not-so-helpful strategies like distractions or turning to alcohol.
Our metacognitive beliefs activate unhelpful thinking styles in response to thoughts, feelings, and impulses that show up.
Why is it important to change metacognitive beliefs in therapy?
Correcting unhelpful metacognitive beliefs is very important in MCT. These beliefs act like the control center, influencing the Cognitive Attentional Syndrome (CAS) which includes counterproductive thinking patterns like constant worry and rumination.
This loop of overthinking often sustains mental disorders like anxiety, depression, OCD, social phobia, and low self-esteem. Therefore, adjusting these beliefs plays a critical role in disrupting this cycle and promoting better mental well-being.
What is self-regulation?
According to Wells (5), our mind is constantly engaged in self-regulation, routinely processing negative thoughts, emotions, and disappointments, which is similar to how the body can mend a broken arm. Thoughts, mental images, and impulses naturally come and go fleetingly. However, when we latch onto them by excessive rumination, worry, (or through other CAS strategies), we disrupt this inherent self-regulation.
The primary goal of MCT is to facilitate this self-regulation, allowing individuals to heal from mental disorders.
Self-regulation is a natural ability that happens without our help.

How can MCT help me recover from mental illness?
The below steps are very important in MCT treatment of mental disorders:
- Reducing unhelpful strategies like rumination, worry, thought monitoring, and thought suppression through strategies like detached mindfulness and worry postponement
- Changing metacognitive beliefs through verbal dialouge and metacognitive experiments in the sessions (from “I can’t control ruminations” to “I have full control over worrying/rumination”)
- Using attention flexibly through the attention training technique (so that you choose what you want to pay attention to in a situation)
When I start working with a new client, my main goal is to make them realize they have a real say in how their mind operates, even if they can’t control every single thought. We usually spend much of our time talking about how they think, not just what thoughts come up. To make this process engaging, we conduct hands-on, eye-opening experiments during our sessions. This is to equip them with newer and better strategies that will help them navigate their mental landscape with more confidence and influence.
To heal from mental disorders, reducing the CAS and adopting the belief that you can regulate your worrying and overthinking is vital. A skilled MCT therapist plays a crucial role in facilitating this process.
MCT self-help – can I benefit from MCT on my own?
It is possible to learn how to reduce rumination and worry independently(12) and you can start by following the steps outlined below. However, based on my experience as a practitioner, I have observed that many people misinterpret MCT “techniques”(11) and misuse them without proper guidance from a skilled therapist. Even some newer MCT practitioners can struggle to grasp MCT fully due to its distinctive nature.
Can you be your own therapist? Find out here.
Implementing MCT should ideally feel light and relaxed. If you find yourself struggling during the application on your own, it is likely that how you are applying it needs adjustment. An experienced MCT therapist is very important in refining your practice.
Here is a way you can practice reducing rumination and worry on your own:
- Identify worry and rumination: Pay close attention to your mind whenever you experience a negative shift in your mood. This serves as a cue that you may be overthinking.
- Recognize that it is not helpful to continue worrying and ruminating and decide to stop.
- Refocus your attention on what you are doing
Is Metacognitive therapy another type of Cognitive therapy?
Although MCT deals with cognition (which means thinking), MCT is not just another layer on top of Cognitive-behavioral therapies (CBT) and not the same thing(3).
Cognitive-behavioral therapy (CBT) views negative thoughts as the reason why people develop anxiety and depression. However, everyone has negative thoughts and CBT can’t answer the question of why some people can dismiss negative thoughts naturally, while others get anxiety and depression (10). The theory behind MCT, however, answers this question by underlining the role of metacognitive beliefs in how much people pay attention to their negative thoughts.
The science behind MCT
Metacognitive therapy is supported by a lot of research (6). There is clear evidence of the effects of CAS and the importance of metacognition. Data(7) shows that when people reduce rumination and worry, they recover from mental issues like anxiety, depression, OCD, and even low self-esteem.
Metacognitive therapy can create more changes in thinking than cognitive behavioral therapy, CBT (8) (9). This is consistent across a range of anxiety, mood, psychotic, and addiction-related disorders.
Summary
- Extended thinking styles like rumination and worry contribute to psychological symptoms.
- Metacognitive therapy helps to reduce rumination and worry through specifically designed techniques
- Metacognitive beliefs lie beneath unhelpful thinking styles and should be changed in therapy to ensure long-term outcome
Sources
- Wells, A., & Matthews, G. (1994). Attention and emotion: A clinical perspective. Lawrence Erlbaum Associates, Inc.
- Wells, A., & Matthews, G. (1996). Modelling cognition in emotional disorder: The S-REF model. Behaviour Research and Therapy, 34(11-12), 881–888. https://doi.org/10.1016/S0005-7967(96)00050-2
- Lora Capobianco, Henrik Nordahl (2022) A Brief History of Metacognitive Therapy: From Cognitive Science to Clinical Practice. Cognitive and Behavioral Practice, Available online at www.sciencedirect.com
- Wells, A., (2009). Metacognitive therapy for anxiety and depression. Guilford press.
- Wells A, Capobianco L, Matthews G and Nordahl HM (2020) Editorial: Metacognitive Therapy: Science and Practice of a Paradigm. Front. Psychol. 11:576210. doi: 10.3389/fpsyg.2020.576210
- Normann & Morina, The Efficacy of Metacognitive Therapy: A Systematic Review and Meta-Analysis, Front. Psychol., 14 November 2018 | https://doi.org/10.3389/fpsyg.2018.02211
- Solem, S., Wells, A., Kennair, L. E. O., Hagen, R., Nordahl, H., & Hjemdal, O. (2021). Metacognitive therapy versus cognitive–behavioral therapy in adults with generalized anxiety disorder: A 9-year follow-up study. Brain and Behavior, 11, e2358. https://doi.org/10.1002/brb3.2358
- Callesen, P., Reeves, D., Heal, C. et al. Metacognitive Therapy versus Cognitive Behaviour Therapy in Adults with Major Depression: A Parallel Single-Blind Randomised Trial. Sci Rep 10, 7878 (2020). https://doi.org/10.1038/s41598-020-64577-1
- Fisher, P., & Wells, A. (2009). Metacognitive therapy: Distinctive features. Routledge/Taylor & Francis Group.
- Wells A (2019) Breaking the Cybernetic Code: Understanding and Treating the Human Metacognitive Control System to Enhance Mental Health. Front. Psychol. 10:2621. doi: 10.3389/fpsyg.2019.02621
- These are better described as strategies rather than techniques. Techniques often involve taking specific actions, but in the case of most MCT exercises, they revolve around the idea of not taking action or simply doing nothing.
- Wells A, Reeves D, Heal C, Fisher P, Doherty P, Davies L, Heagerty A, Capobianco L. Metacognitive therapy self-help for anxiety-depression: Single-blind randomized feasibility trial in cardiovascular disease. Health Psychol. 2022 May;41(5):366-377. doi: 10.1037/hea0001168. PMID: 35467904; PMCID: PMC9037049.



