Metacognitive therapy (MCT) is a relatively recent psychological therapy compared to the golden standard treatment for the past 50 years: Cognitive behavioral therapy (CBT). Both approaches focus on thinking, however,
MCT and CBT are very different. MCT aims to reduce thinking processes like rumination and worry and change the metacognitive beliefs responsible for activating them. CBT focuses on changing the content of thoughts and doesn’t recognize the role of metacognitive beliefs in mental disorders.
Contrary to CBT, which views rumination and worry as involuntary symptoms of mental disorders, rumination and worry can be reduced and controlled, according to MCT. Rumination and worry are activated by metacognitive beliefs, which is thinking about thinking.
Here is the difference between MCT and CBT explained in more detail.
CBT focuses on the content of thinking. MCT focuses on thinking about thinking
1. MCT and CBT are built on different theories of mental disorders
The theory behind MCT
Metacognitive therapy (MCT) is built on a theory called the S-REF model (Self-Regulatory Executive Function model and later the Metacognitive Control system (MCS)) through the work of Adrian Wells, a British professor in psychology.
According to the MCS theory, there are two different thinking systems in the brain, the MCS (where metacognitive knowledge is stored) and the CS (cognitive system, where thinking happens).
The MCS monitors and controls how we think (for example, whether we ruminate about problems in the CS). It also affects the neural network (for example, gut feeling, inhibition, arousal, and reward).
The CS, on the other hand, is where thinking happens (rumination, worry, thought suppression, daydreaming, etc.).
Based on this understanding of the mind, what we think about (the content of thoughts) is not really important in causing mental disorders like anxiety and depression. Instead, how we think and what we believe about the way we think is much more important.
According to the theory behind MCT, the psyche can heal itself from distressing thoughts and feelings. Just like the way the body can heal a broken arm, the mind has the ability to recover from depression, anxiety, low self-esteem, and even from traumatic events on its own.
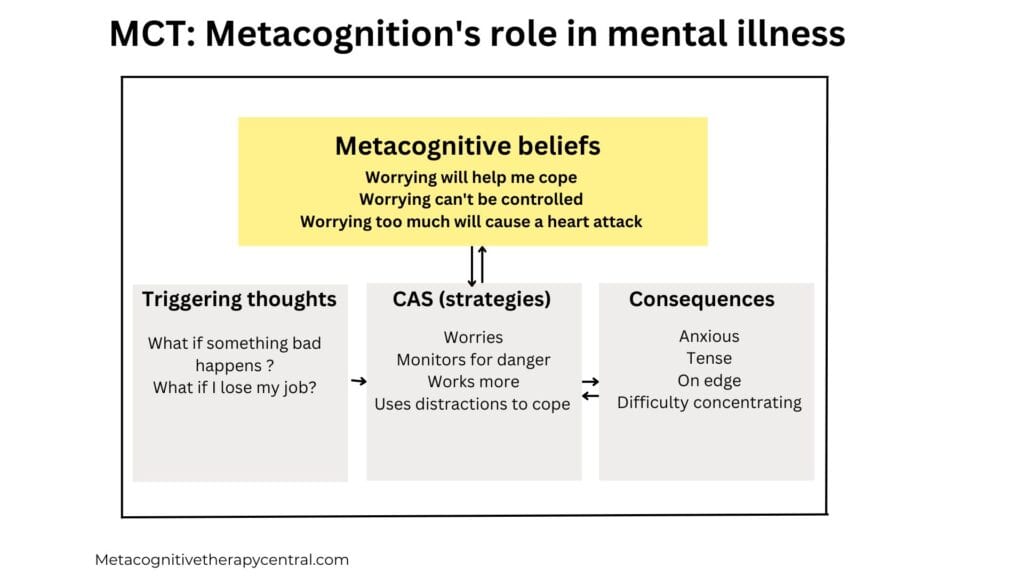
Thoughts, images, and impulses come up in the mind shortly but will disappear again on their own. Therefore, according to MCT, psychological illness is not caused by brief thoughts or feelings. Instead, psychological illness like depression, anxiety, and OCD, for example, is caused by unhelpful coping strategies that people use when they have negative thoughts and feelings (1).
These unhelpful coping strategies are called the CAS (the Cognitive Attentional Syndrome), and consist of:
- Rumination
- Worry
- Threat monitoring
- Other unhelpful coping strategies (alcohol, seeking reassurance, or suppressing thoughts).
Holding on to unwanted thoughts and feelings through the CAS, we hinder the mind from regulating itself. And that’s when thoughts and feelings persist for a longer time. According to Metacognitive therapy, CAS is the reason behind psychological illness.
The goal of MCT is to help patients reduce the CAS and change false metacognitive beliefs bout thinking, like:
I can’t stop worrying
Rumination is helpful in finding solutions to problems
Worrying can make me lose my mind
Metacognitive therapy is supported by a lot of research (2). There is clear evidence that CAS is the problem behind mental disorders. Therefore, when people reduce rumination and worry (and other unhelpful coping strategies), they recover from mental illnesses like anxiety, depression, OCD, and even low self-esteem.
MCT states that the negative thoughts and feelings are brief and not problematic. Worrying and ruminating about them for a long time is what creates psychological problems.
The theory behind CBT
Cognitive-behavioral therapy (CBT) is originally based on the work of Aaron T. Beck, an American psychiatrist. Beck’s CBT is based on clinical observations in his patients and then described through cognitive psychology (the scientific study of attention, language use, memory, perception, problem-solving, and creativity) and behavioral psychology (understanding the behavior and learning of humans and other animals).
CBT states that psychological disorders are maintained by:
- Negative thoughts
- Cognitive distortions, which are errors in logical thinking (like black and white thinking, “I always fail” and “everyone is out to get me“)
- General beliefs about the world, the self, and the future (“I am unworthy,” “the world is a dangerous place“)
The cognitive-behavioral model theorizes that the way we think and behave influences our emotional well-being. These cognitive distortions and beliefs lead people to experience negative thoughts in specific situations. CBT, therefore, aims to challenge and change negative thoughts and beliefs and help patients replace them with realistic thoughts.
The overall goal of treatment is reducing symptoms, improving functioning, and achieve remission of mental illness. To achieve this goal, the patient and therapist participate in a collaborative problem-solving process to test and challenge the validity of negative thoughts and maladaptive behavioral patterns.
CBT is one of the most researched psychological therapies with over 80,000 articles showing that CBT has a moderate effect on depression and effective in the treatment of some anxiety disorders (3).
In recent years, therapists have been mixing techniques from different therapeutic treatments with CBT, for example, mindfulness techniques. This makes it harder to measure CBT’s exact effect because no standardized CBT manual exists to treat mental illness (4).
2. MCT focuses on metacognition – CBT focuses on cognition
Metacognitive beliefs are beliefs about thinking. According to MCT, metacognitive beliefs lead to unhelpful thinking patterns (worry, rumination, thought suppression, avoidance, reassurance seeking) in order to tackle painful thoughts, feelings, and impulses.
Examples of metacognitive beliefs are:
“I should ruminate to find solutions”
” It is helpful to worry about my problems”
“I can’t control my rumination”
“Worrying makes me go crazy”
If anxious or depressed patients have negative metacognitive beliefs (“I can’t control ruminations. I am going crazy with all this thinking”), they don’t believe that they have a choice but to ruminate and worry. So they keep ruminating for hours and days and end up feeling worse because rumination and worry prolong negative feelings.
False and unchanged metacognitive beliefs like the ones above lead to unhelpful thinking patterns and other more unhelpful strategies like alcohol, distraction, avoidance, fights, etc.)
In therapy sessions, MCT focuses on changing metacognitive beliefs, both verbally and through experiments (for example, by making the patient worry uncontrollably in the session to see whether they can stop again, which proves that worrying can be controlled).
Changing the patient’s metacognitive beliefs in therapy will lead to reduced worry and rumination, which allows the mind to self-regulate.

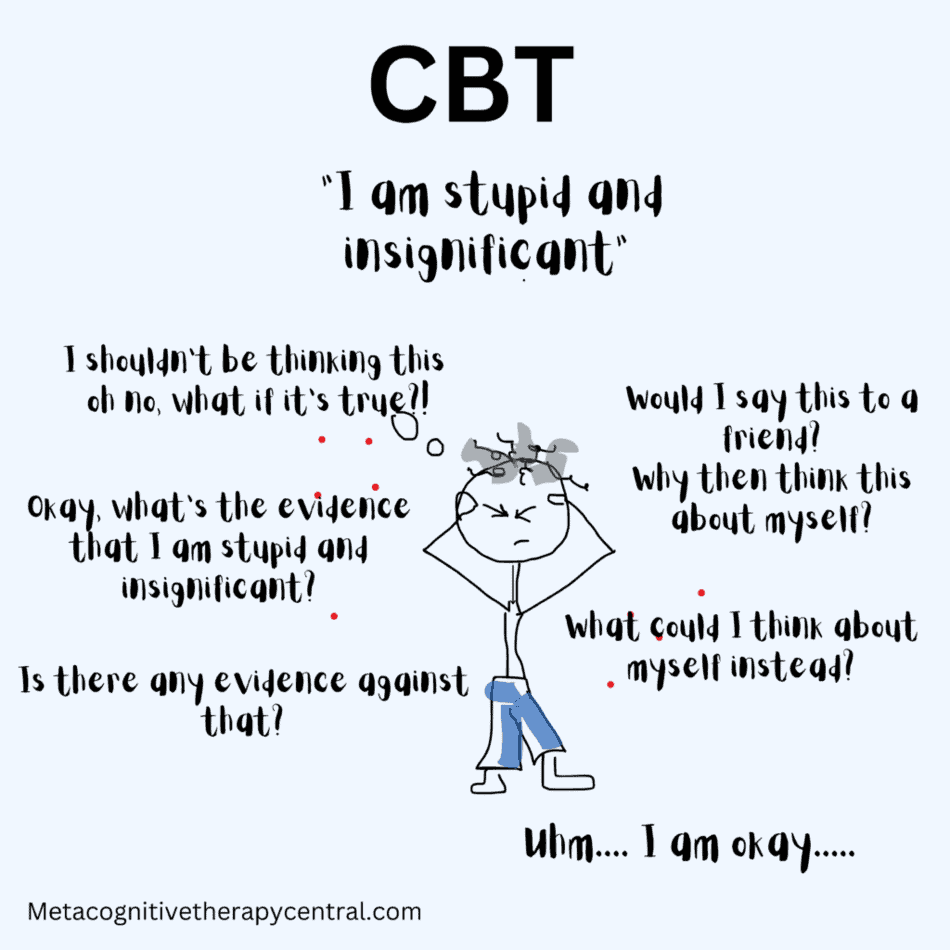
CBT, on the other hand, doesn’t recognize metacognitive beliefs or aims at changing them. Instead, the focus is on cognition (thinking) and not metacognition (thinking about thinking).
CBT uses different strategies to challenge the content of the patient’s negative thoughts: restructuring thoughts (finding the evidence for and against the negative thought), identifying and changing cognitive distortions ( for example changing “being wrong is unacceptable” to “it’s okay to make mistakes“), problem-solving (for example, learning how to have a conversation instead of avoiding them).
In this post, you can read more about the difference between MCT and CBT for anxiety.
The focus of treatment in CBT is to challenge and change what patients think (for example, changing the thought “I am stupid“) because that is believed to cause mental disorders.
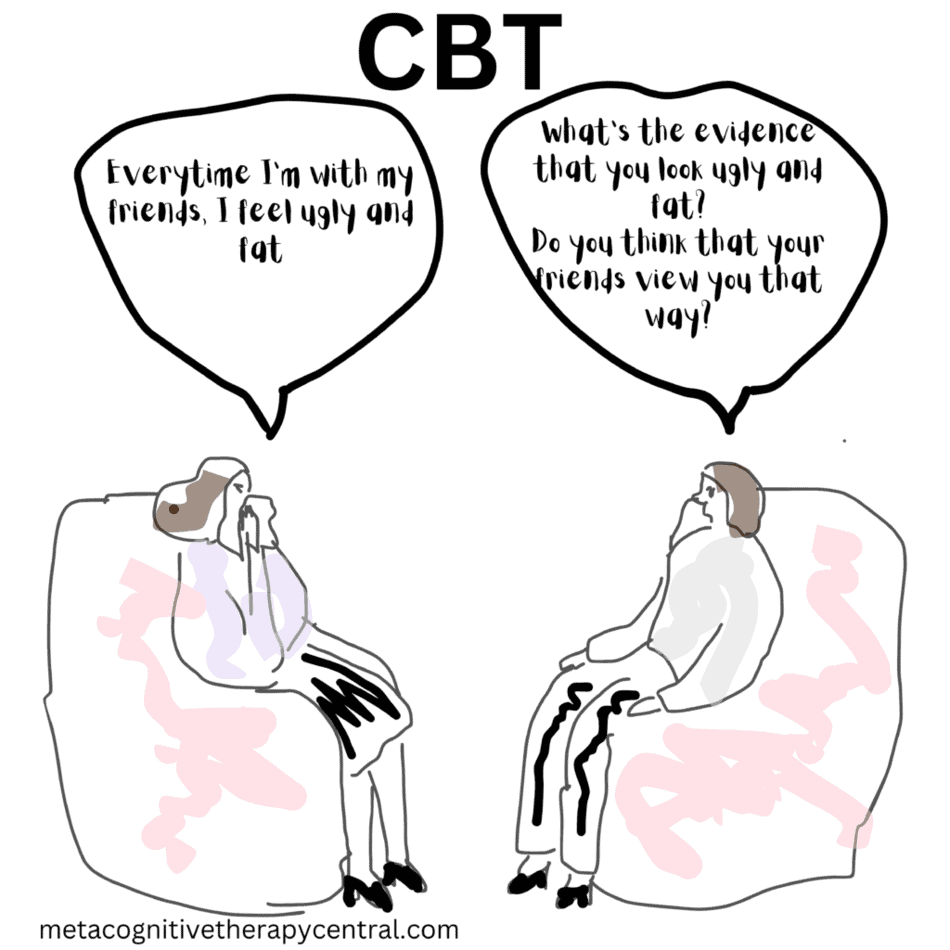
A cognitive-behavioral therapist will ask her patient the following:
“Thinking that you are a failure, what is the evidence for that? Is there any counter-evidence?“
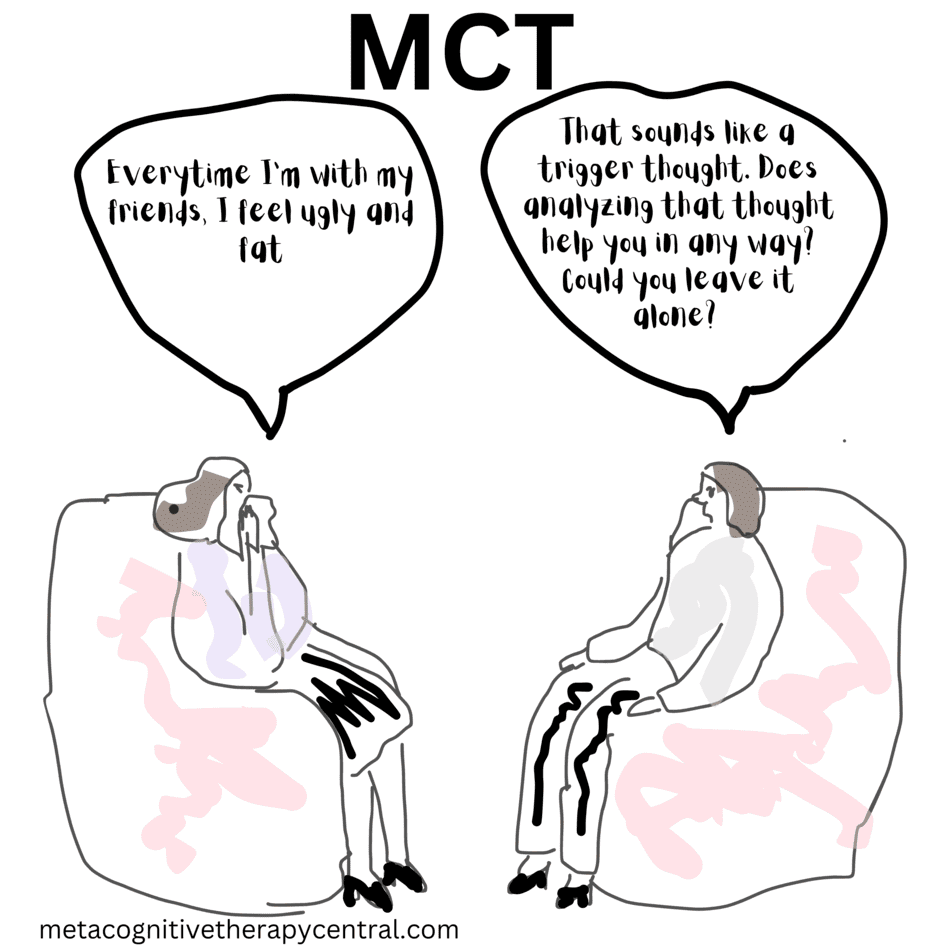
A metacognitive therapist will ask her patient the following:
“When the thought ‘I am a failure’ comes up, what do you do with it? Do you hold on to it, ruminate about it? Has it helped you feel better?“
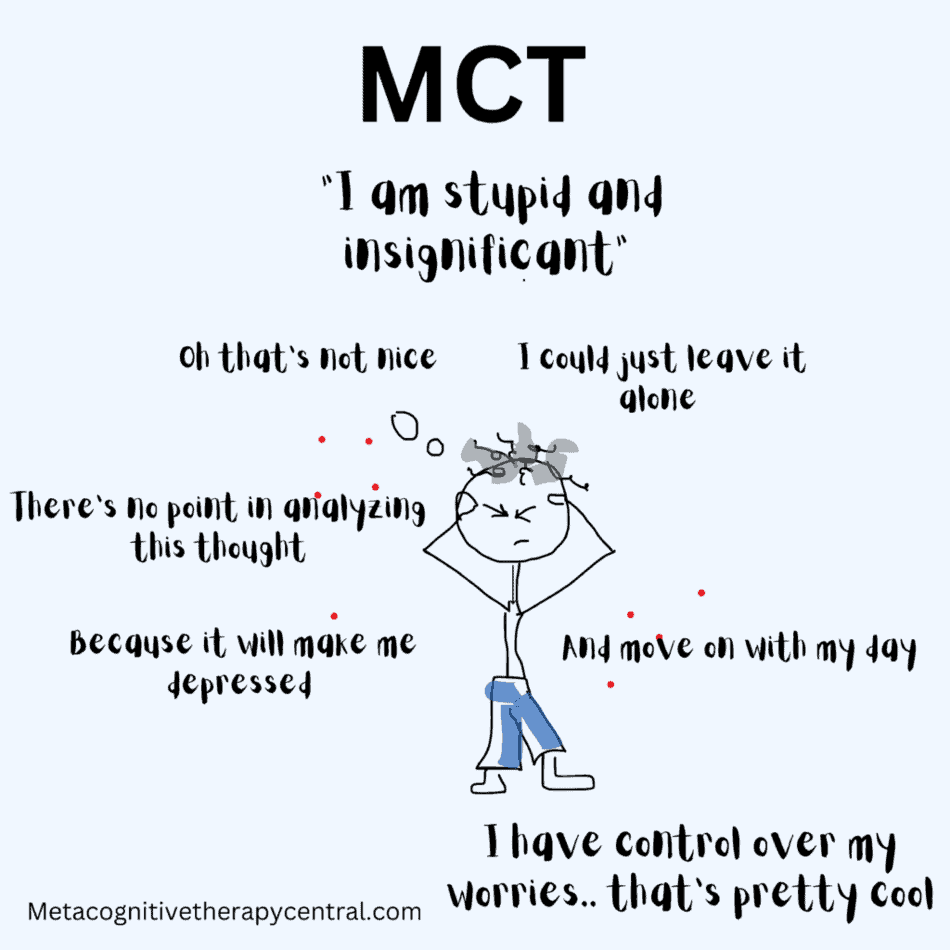
3. In MCT thoughts don’t matter – In CBT thoughts cause mental disorders

The mind is constantly hit by impulses, thoughts, and feelings. These thoughts and feelings come from an unconscious level that is reflexive and automatic, and we don’t have much control over them. We can’t control what kinds of thoughts enter the mind.
The brain produces around 60 thousand thoughts every day. These thoughts are a mix of positive, negative, and neutral thoughts.
Thoughts like “I am looking forward to the weekend” or “I am a failure” appear spontaneously from the experiences that we have every day. But, they are brief, and they will disappear by themselves if we don’t ruminate about them.
MCT doesn’t view thoughts as significant or harmful because of their transient nature. Therefore, there is no point in changing the content of thoughts and therapy focuses on teaching patients to cultivate a relaxed relationship with negative thoughts. This happens by letting thoughts come and go on their own and allowing the mind to take care of them.
CBT views thoughts as important and the driver of mental disorders like anxiety and depression, and places therefore great emphasis on challenging and changing them in therapy. Thoughts are not viewed as brief inner events like they are in MCT, but instead as significant for functioning.
For example, if someone has the thought, “I look fat” MCT will show them how they can still have the thought and go out on a date, while CBT would try to change the thought first.
4. MCT facilitates problem-solving indirectly – CBT problem-solves directly
There is a difference between ruminating about a problem and problem-solving. The former consists of a lot of thinking whereas the latter explicitly works toward a concrete solution. An important part of CBT is also to help patients solve problems in therapy. But these problems are probably caused by excessive rumination and worry, according to MCT, and they could be easily solved if the patient stopped worrying and ruminating so much.
MCT facilitates indirect problem-solving through the reduction of worry and rumination. Usually, the patients know how to go about solving a problem and they don’t necessarily need to learn that in therapy. According to some research, reducing worry helps gain better problem-solving abilities (5).
For example, CBT teaches patients with social anxiety how to interact socially through rehearsing lines and role-playing conversations. MCT assumes that the patient inherently knows how to interact, and instead focuses on removing barriers that get in the way of doing so (rumination, worry, and exaggerated self-focus).
5. MCT uses exposure to change metacognitive beliefs – CBT uses exposure to reduce anxiety
CBT exposes patients to feared situations in an attempt to make them habituate to the anxiety ( to help the patient tolerate the anxiety and let the brain regulate the emotions so that the anxiety dissipates). The goal of exposure in CBT is to reduce the level of anxiety.
Whether the exposure is successful depends on how much anxiety the patient feels each time they get into the feared situation, but the process can be time-consuming and draining for the patient.
MCT does expose patients to feared situations, but the goal is to demonstrate that the patient can act despite anxiety. This helps change metacognitive beliefs (for example, that the patient can’t lose control over worrying or that they can control what they pay attention to despite feeling anxious).
Summary
- MCT and CBT are very different therapeutic approaches.
- MCT focuses on incorrect ways people think about thoughts (Metacognitive beliefs) and the goal is to change these beliefs so that rumination and worry can be reduced.
- CBT aims to change the content of negative thoughts to more realistic thinking and through problem-solving to help reduce emotional distress.
- MCT works on a metacognitive level, whereas CBT works on a content level.
References
- Wells, A. & Matthews, G. (1996). Modelling cognition in emotional disorder: The S-REF model. Behaviour Research and Therapy. 34. 881-888. 10.1016/S0005-7967(96)00050-2.
- Normann & Morina, The Efficacy of Metacognitive Therapy: A Systematic Review and Meta-Analysis, Front. Psychol., 14 November 2018 | https://doi.org/10.3389/fpsyg.2018.02211
- Fisher, P. L. (2006). The Efficacy of Psychological Treatments for Generalised Anxiety Disorder? In G. C. L. Davey & A. Wells (Eds.), Worry and its psychological disorders: Theory, assessment and treatment (pp. 359–377). Wiley Publishing. https://doi.org/10.1002/9780470713143.ch20
- Schweiger JI, Kahl KG, Klein JP, Sipos V and Schweiger U (2019) Innovation in Psychotherapy, Challenges, and Opportunities: An Opinion Paper. Front. Psychol. 10:495. doi:10.3389/fpsyg.2019.00495
- Wells, A., & Matthews, G. (1994). Attention and emotion: A clinical perspective. Lawrence Erlbaum Associates, Inc.
- Carr, Alan & McNulty, Muireann. (2016). Handbook of Adult Clinical Psychology: An Evidence-Based Practice Approach.
- Wells A (2019) Breaking the Cybernetic Code: Understanding and Treating the Human Metacognitive Control System to Enhance Mental Health. Front. Psychol. 10:2621. doi: 10.3389/fpsyg.2019.02621