Mental disorders are prevalent i many different countries and that the number of people meeting diagnostic criteria for a mental disorder appears steeply growing. Current psychological treatments show only a medium effect (around 50% recovery), while the relapse rates are high (3). There is therefore a need for effective mental health treatments.
Studies have found that MCT can significantly reduce symptoms and improve functioning in patients with anxiety, depression, and OCD. Randomized controlled trials of anxiety and depression show 72–80% recovery rates for MCT, which is very high compared to standard treatments like Cognitive-behavioral therapy (CBT) (2).
Besides, MCT has proven effective for social anxiety, and it is a recommended intervention in the health guidelines, which are evidence-based recommendations for health and care in England (12).
Metacognitive therapy (MCT) has been effective in treating various mental health problems, including depression, anxiety, and OCD. MCT is developed by professor Adrian Wells, whose research clearly highlights the mechanisms that maintain psychological disorders.
What makes MCT an effective treatment?
The main reasons why MCT is an effective mental health treatment are the following:
- MCT’s strong theoretical background
- MCT reduces unhelpful thinking styles like rumination and worry
- MCT challenges false metacognitive beliefs about thinking (metacognitive beliefs are beliefs about thinking, for example, that rumination is helpful or that worry is uncontrollable).
Go to this post for a comprehensive overview of the research showing the effect of MCT
1. MCT has a strong theoretical background
Metacognitive therapy is built on an empirically grounded theory, (called the S-REF model and later developed as the Metacognitive Control System Model). This theory clearly identifies the underlying mechanisms that maintain mental disorders like anxiety, depression, and OCD.
These mechanisms are called uncontrollable rumination and worry (a type of overthinking that becomes pervasive and uncontrollable) that maintain negative emotions like anxiety, stress, and sadness. This can then lead to activating unhelpful coping strategies like paying too much attention to “threats,” suppressing emotions, and avoidance, which only work as a short-term relief from negative thoughts.
According to MCT, the reason behind mental disorders is that people ruminate and worry about their problems for extended periods, and at some point, feel that rumination and worry get out of their control.
MCT doesn’t combine techniques from treatments
Contrary to most other psychological treatments, MCT avoids combining techniques from different psychological treatments, which is, for example, the case with Mindfulness-based CBT (a combination of CBT and Mindfulness). That way, it is easier to measure what part of the treatment actually works.
When psychological treatments combine different techniques, it not only gets harder to measure which technique works, but it is also harder to understand what makes people mentally ill in the first place (6).
2. MCT effectively reduces rumination and worry
Metacognitive therapy is one of the few psychological therapies that directly identifies that worry and rumination cause and maintain mental illness, and treatment, therefore, focuses on reducing these.
Rumination and worry are repetitive thinking styles (7), and, according to MCT, cause emotional distress if not controlled.
Rumination is usually thinking about past problems
Worry is thinking about future situations
When people ruminate, they typically ask themselves a lot of “why” questions: “Why did I behave that way?“, “Why have I been feeling so low lately?“.
Worrying is often initiated by asking “what if” questions: “What if I have a serious illness?“, “What if I can’t handle all the pressure at work?”
Worry and rumination are usually not the best ways to find solutions to problems (8). Prolonged worry and rumination exacerbate negative emotions and physiological symptoms like dizziness, restlessness, anxiety, and sadness.
If someone experiences a low mood, ruminating about it to find out why they feel this way will usually make them feel worse after some time. This is also the case when someone worries about catastrophic scenarios. Worrying makes them focus more on how anxious they feel and how terrible things will be if their worries came true.
It is, therefore, important to help patients reduce worry and rumination that has gotten out of control. Worry and rumination can be reduced through specially developed techniques like detached mindfulness, developed by professor Wells.
According to MCT, extended worry and rumination prolong negative emotions (and have other negative consequences) and cause depression and anxiety (9).
3. MCT challenges beliefs about thinking
An important part of Metacognitive therapy is to identify beliefs about thinking and change them to more accurate beliefs. Challenging beliefs about thinking will help reduce worry and rumination and help people recover from mental disorders (14).
When rumination and worry get out of control (for example, when people worry uncontrollably for many hours every day), it is because a metacognitive belief about thinking has been activated:
I can’t stop worrying
Rumination is out of my control
Beliefs about how we think are called metacognitive beliefs. People suffering from extended worry and rumination usually believe they can’t stop. According to Wells, they have uncontrollability metacognitive beliefs.
If someone doesn’t believe in their ability to stop ruminating, they will either continue to ruminate or try to cope with rumination through avoidance, drinking alcohol, or using distractions. Usually, coping strategies backfire and make people feel even worse long-term (7).
In MCT, metacognitive beliefs are the focal point of therapy, and they are changed through experiments like worry postponement.
If the patients’ metacognitive beliefs are not challenged, they will fall back into uncontrollable worry and rumination at some point in the future. Therefore, challenging metacognitive beliefs is also important to prevent relapse into mental illness. Studies show that the relapse rates for people with anxiety and depression are lower after treatment with MCT than with CBT (10).
Is MCT better than CBT?

Results from a meta-analysis (a statistical analysis that combines the results of multiple scientific studies on the same topic) suggest that MCT may be more effective than CBT (2).
Results from a 2020 study comparing MCT to CBT for depression proved that MCT was more effective in treating depression (11).
A study from 2021 collected 9-year follow-up data of patients who either received group CBT or group MCT for generalized anxiety disorder. They found that the relapse rates were higher for those patients who received CBT (almost one out of four patients developed anxiety again):
- In the CBT group, 23.1% were re-diagnosed with generalized anxiety disorder.
- In the MCT group, 9.5% were re-diagnosed with generalized anxiety disorder.
Research has shown that MCT is an effective treatment for generalized anxiety disorder (GAD) and has better results than CBT. This is an important finding because GAD is one of the most frequent anxiety disorders seen in primary care patients (22% who seek their general physician suffer from generalized anxiety). GAD impairs social functioning, and there is a great need for quality treatment.
Several published studies have tested the effects of MCT in treating Generalized anxiety disorder (GAD), which seems to be a good treatment for reducing GAD symptoms. MCT for GAD has also been compared with CBT for GAD, and the results show that MCT shows better recovery rates for GAD than CBT. Clinical studies show that 65% of GAD patients recover after MCT compared with 38% after CBT (4).
Why is MCT more effective than CBT?
There are several reasons why MCT might be a better treatment for anxiety and depression than CBT.
1) CBT gives places importance on negative thoughts (negative thoughts and beliefs about oneself or the world cause mental illness); however, little importance is given to worry and rumination (which is proven by research to cause mental illness).
2) CBT does not focus on modifying metacognitive beliefs. Since metacognitive beliefs are the drivers of worry and rumination according to research (7) (9) (13) (14), challenging the content of thoughts may not produce a sustainable positive outcome as it would if worry and rumination were reduced.
Studies have shown that changing metacognitive beliefs (which is the focus of MCT) predicts better results for patients with OCD, compared to only challenging the content of their intrusive thoughts (13).
To confirm these results, there is a need for more and larger studies that include more people. You can read more about scientific studies and criticism of MCT in this post.
CBT challenges the content of thoughts: “My hands are contaminated with bacteria” MCT challenges the belief about the thought, “Thinking this makes it true.”
Read this post to learn more about the differences between MCT and CBT.
MCT research overview
MCT is recognized as one of the best available treatments for anxiety
People with Generalized anxiety disorder (GAD) have a higher risk of developing depression, alcohol and benzodiazepine dependency, and somatoform disorders (a form of mental illness that causes one or more bodily symptoms, including pain). Most patients struggle with GAD for 8–10 years, with low recovery rates even when treated. This is the reason that GAD is viewed as a chronic disorder.
MCT has shown very promising results for GAD. Here is an overview of the studies of MCT for GAD:
| Who did the study? | What did they study? | Results | Specific changes that happened |
| Wells & King, 2006 Link to study | Uncontrolled trial 10 patients with GAD received MCT for 4-12 sessions 50% of the patients had another diagnosis as well | 87% of patients recovered as assessed from anxiety, and 75% remained recovered at six and 12-month follow-up | Improvements in anxiety symptoms, worry, and depressive symptoms |
| Wells, A., Welford, M., King, P., Papageorgiou, C.,Wisely, J., & Mendel, E. 2010 Link to study | A pilot randomized trial of Metacognitive therapy vs. applied relaxation (AR) in adults with GAD. 20 patients received 8-12 sessions of either MCT or Applied relaxation. | 80% improved because of MCT 10% improved because of AR. MCT proved better on all measures compared to AR. MCT maintained superiority over AR on almost most measures at 12-month follow-up. | |
| Van der Heiden, C., Muris, P., & Van der Molen, H. T. 2012 Link to study | A randomized controlled trial comparing Metacognitive therapy and Intolerance of uncertainty therapy (IUT) 61 patients received MCT, 60 patients received Intolerance of uncertainty treatment (IUT) | Both treatments made significant improvements in worry and anxiety symptoms and depression. 72% recovered through MCT, 48% recovered through IUT MCT significantly changed the patients’ metacognitive beliefs compared to IUT. | Both treatments reduced intolerance of uncertainty, negative metacognitive beliefs, and positive metacognitive beliefs about worrying. |
| Svein Haseth, Stian Solem, Grethe Baardsen Sørø, Eirin Bjørnstad, Torun Grøtte, and Peter Fisher 2019 Link to study | Group Metacognitive Therapy for Generalized anxiety disorder: A pilot feasibility trial | 65.3% were recovered 30.4% were improved 4.3% showed no change. Recovery rates raised to 78.3% after three months follow-up. These recovery rates were regardless of the number of patients’ diagnoses. MCT was associated with significant reductions in worry, anxiety, depression, metacognitive beliefs, and maladaptive coping. | Reducing worry Reducing maladaptive coping behaviors Changing metacognitive beliefs |
| Hans M Nordahl, Thomas D Borkovec, Roger Hagen, Leif E O Kennair, Odin Hjemdal, Stian Solem, Bjarne Hansen, Svein Haseth, Adrian Wells Link to study | A randomized controlled study comparing Metacognitive therapy with the gold standard treatment, CBT, in patients with GAD. The study controlled for non-specific factors. | 65% recovered after MCT and 38% after CBT. MCT had better outcomes than CBT on most comparisons. The results were independent of non-specific treatment factors, proving that the treatment itself was effective. | CBT and MCT reduced worry and anxiety symptoms both in the short- and long term. |
70-80% of patients recover from generalized anxiety disorder with MCT. The recovery rates are maintained up to 30 months after treatment.
How does MCT work in the brain?
The exact way that MCT affects the brain is still to be researched. In general, the effect of psychotherapy on the nervous system is still unclear, making it difficult to point out how therapy works.
However, emerging new theories about the brain can help us understand how MCT might work and why it is effective.
In 2019, Adrian Wells, the founder of MCT, came up with a theory of how MCT affects the brain. The theory is called the metacognitive control system (MCS). It explains that there are two different thinking systems in the brain, the MCS (where metacognitive knowledge is stored) and the CS (cognitive system, where thinking happens) 14.
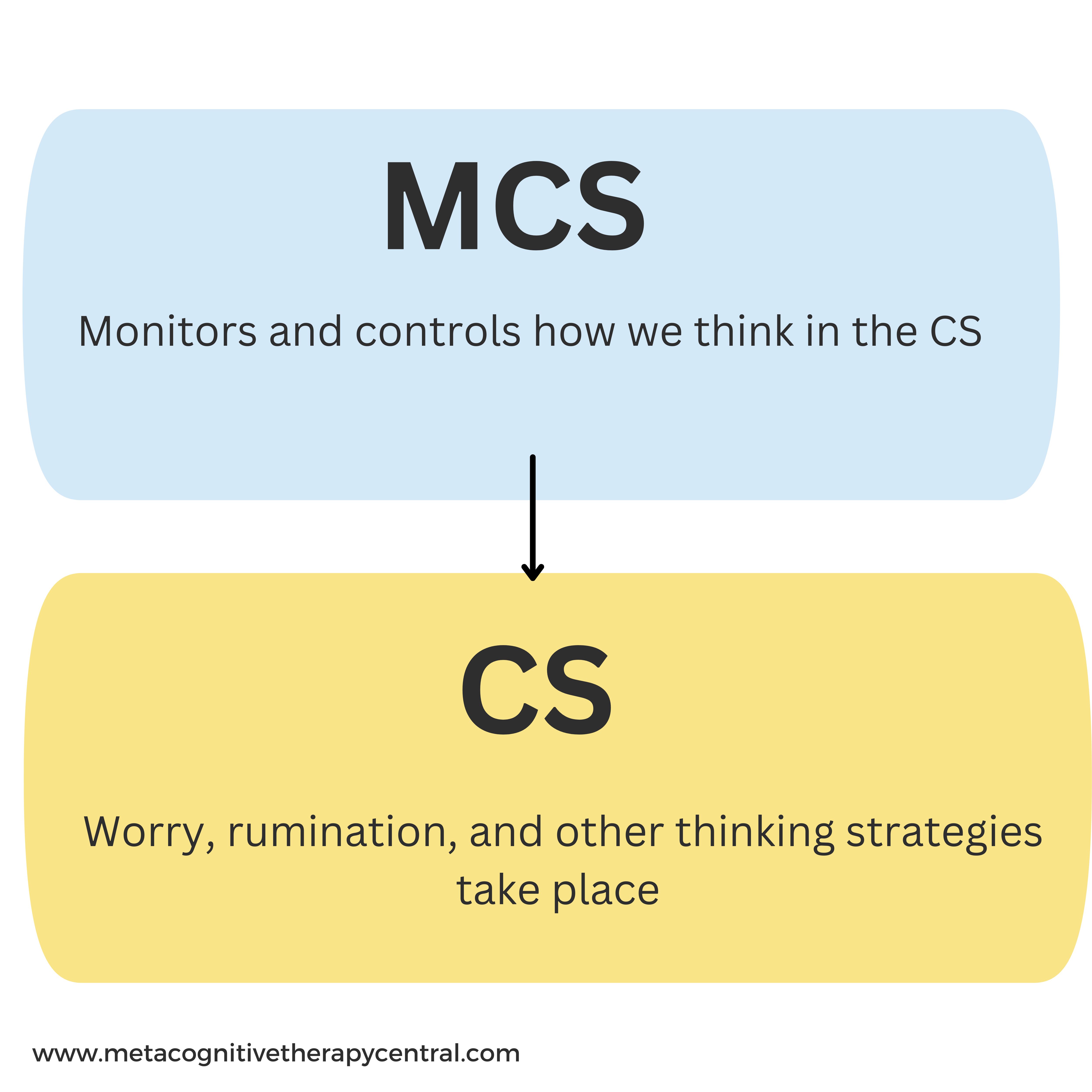
The MCS monitors and controls how we think (for example, whether we ruminate about problems in the CS). It also affects the neural network (for example, gut feeling, inhibition, arousal, and reward).
The CS, on the other hand, is where thinking happens (rumination, worry, thought suppression, daydreaming, etc.).
How the two systems communicate
The MCS monitors and controls what happens in the CS (for example, whether one should think more about a negative thought or not). The MCS has a “standard manual” for how someone should think in the CS. For example, if the manual contains “I must worry to solve my problems,” then that person activates worrying whenever a negative thought comes up “what if I didn’t turn off the stove?“.
This manual is also called metacognitive information (metacognitive beliefs).
Why is it important to understand the two systems?
Wells’ distinction between these two systems in the brain (the CS and the MCS) is important not only in understanding mental disorders but also in what constitutes effective mental health treatment.
According to Wells, effective mental health treatment should focus on changing the content of the MCS (for example, changing metacognitive beliefs) instead of only changing the content of the CS (for example, changing negative thoughts to realistic thoughts as is the case in cognitive-behavioral therapy).
Modifying the content of MSC will help reduce how much someone worries and reduce the risk of developing a mental disorder. Therefore, MCT works because it modifies the “standard manual” to reduce overthinking.
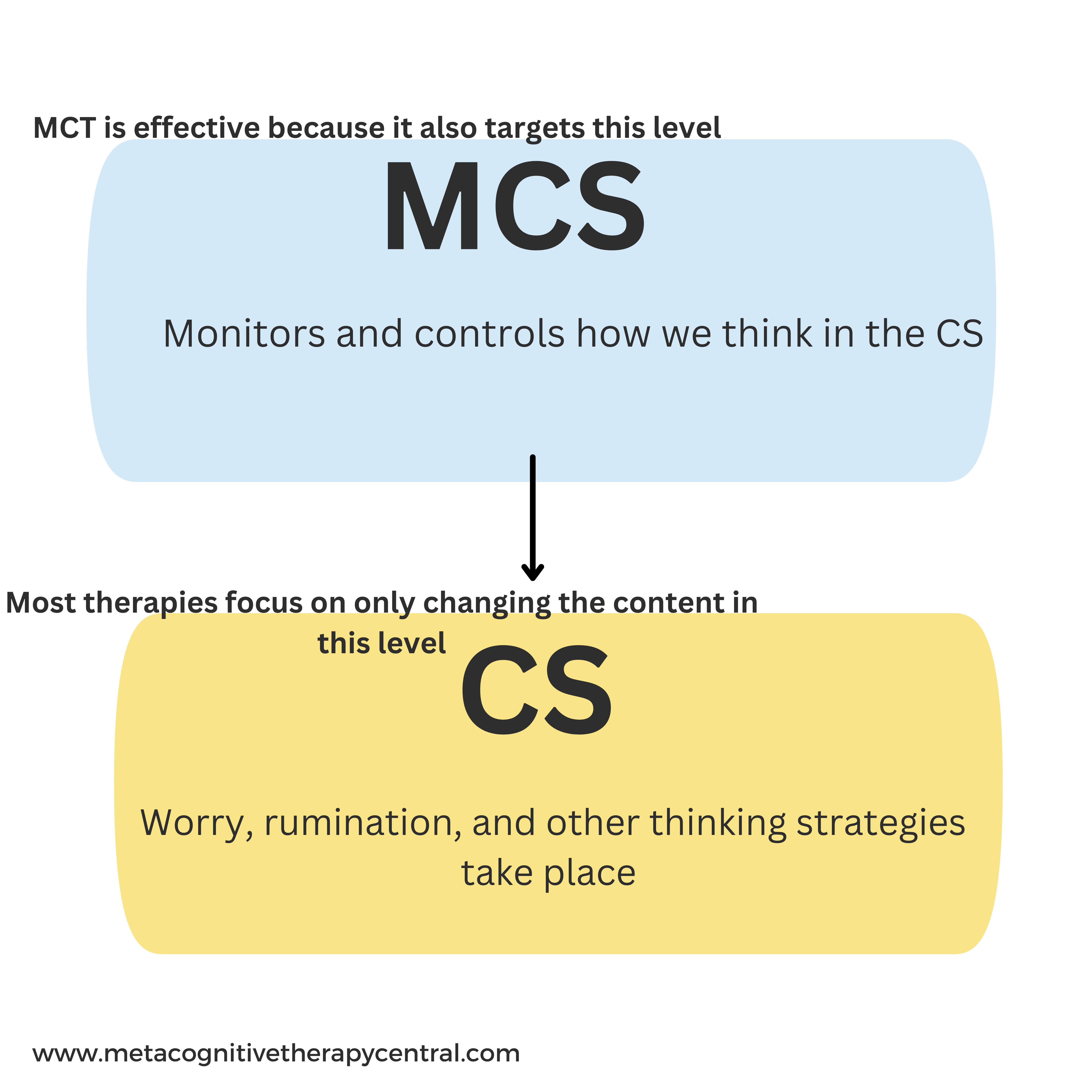
Although this theory is yet to be validated by more research, understanding the MCS theory is a step closer to developing effective psychological treatment while preventing relapse rates. Metacognitive therapy seems promising as an effective mental health treatment. It focuses on modifying metacognitive beliefs and successfully helps people recover from mental disorders like anxiety, depression, and OCD.
According to MCT, Thoughts are not important, but how you relate to them is.
Do patients think that MCT is effective?
There are pros and cons to each type of psychotherapy from the patients’ perspectives. Here is what patients tell us about their experience with MCT:
Pros
It is very simple once you understand the reason. Don’t grab onto negative thoughts unless you want to sustain them.
In Metacognitive therapy, I have learned to disengage from negativity (thoughts, people, and situations). I can’t control other people or the negative thoughts they trigger in me, but I have full control over how I respond to those triggers. That feels very empowering.
I feel less restricted because I no longer avoid things because of anxiety. If I feel anxious, I know that it is not harmful and that I can still function. I can still work, socialize, and play with my son.
I no longer believe that my thoughts come true just because I have them. I wish that I had known this many years ago.
I really believe that I can control my focus 100%. I can engage in conversations and work even when there are distractions.
Thoughts are just thoughts. They come and go, and I choose which ones I want to listen to.
I have had the busiest week ever, but I don’t feel stressed about it because I don’t worry.
I have learned that I can still work on my problems without worrying about them.
Cons
I have been ruminating my whole life. It feels scary to let it go; sometimes, I feel empty without it.
Worrying about others makes me a better person… or I am learning that it’s not necessarily true. But what if I become superficial if I stop worrying?
I have learned that I should allow negative thoughts to enter my mind. That can feel uncomfortable at times compared to suppressing my thoughts.
I am impatient. It takes hard work to change a habit, and sometimes I lose patience.
I find that I easily fall back into ruminating and worrying. I really need to be aware of that, which I often forget.
Sometimes, in anxiety-provoking situations, I still don’t know what to do. Usually, everything happens so fast, so I push negative thoughts away even though I know that I should leave them alone. It really takes a lot of practice to get good at this.
Thinking is something you choose to do to fleeting thoughts that come up in your mind
Become part of the community on Instagram. Ask questions. Get inspired.
References
- Photo by Raimond Klavins
- Normann N, Morina N. The Efficacy of Metacognitive Therapy: A Systematic Review and Meta-Analysis. Front Psychol. 2018 Nov 14;9:2211. doi: 10.3389/fpsyg.2018.02211. PMID: 30487770; PMCID: PMC6246690.
- Johnsen, T. J., & Friborg, O. (2015). The effects of cognitive behavioral therapy as an anti-depressive treatment is falling: A meta-analysis. Psychological Bulletin, 141(4), 747–768. https://doi.org/10.1037/bul0000015
- Nordahl HM, Borkovec TD, Hagen R, Kennair LEO, Hjemdal O, Solem S, Hansen B, Haseth S, Wells A. Metacognitive therapy versus cognitive-behavioural therapy in adults with generalised anxiety disorder. BJPsych Open. 2018 Sep 11;4(5):393-400. doi: 10.1192/bjo.2018.54. PMID: 30294448; PMCID: PMC6171331.
- Photo by Sir Manuel
- Schweiger JI, Kahl KG, Klein JP, Sipos V and Schweiger U (2019) Innovation in Psychotherapy, Challenges, and Opportunities: An Opinion Paper. Front. Psychol. 10:495 doi: 10.3389/fpsyg.2019.00495
- Wells, A. (2009). Metacognitive therapy for anxiety and depression. Guilford Press.
- Nolen-Hoeksema, S. (2004). The response styles theory. In C. Papageorgiou & A. Wells (Eds.), Depressive rumination: Nature, theory, and treatment (pp. 107–124). New York: Wiley.
- Bailey, R., & Wells, A. (2016). The contribution of metacognitive beliefs and dysfunctional illness beliefs in predicting health anxiety: An evaluation of the metacognitive versus the cognitive models. Clinical Psychologist, 20(3), 129–137. https://doi.org/10.1111/cp.12078
- Solem, S., Wells, A., Kennair, L. E. O., Hagen, R., Nordahl, H., & Hjemdal, O. (2021). Metacognitive therapy versus cognitive–behavioral therapy in adults with generalized anxiety disorder: A 9-year follow-up study. Brain and Behavior, 11, e2358. https://doi.org/10.1002/brb3.2358
- Callesen, Pia; Reeves, David; Heal, Calvin; Wells, Adrian (May 2020). “Metacognitive therapy versus cognitive behaviour therapy in adults with major depression: a parallel single-blind randomised trial”. Scientific Reports. 10 (1): 7878. Bibcode:2020NatSR..10.7878C. doi:10.1038/s41598-020-64577-1
- NCCMH (2013). Social anxiety disorder: the NICE guideline on recognition, assessment and treatment. Leicester & London: The British Psychological Society and the Royal College of Psychiatrists (Full Guideline). https://www.nice.org.uk/guidance/cg159/chapter/Recommendations#interventions-for-adults-with-social-anxiety-disorder-2
- Solem, S., Haland, A. T., Vogel, P. A., Hansen, B., and Wells, A. (2009). Change in metacognitions predicts outcome in obsessive-compulsive disorder patients undergoing treatment with exposure and response prevention. Behav. Res. Ther. 47, 301–307. doi: 10.1016/j.brat.2009.01.003
- Wells A (2019) Breaking the Cybernetic Code: Understanding and Treating the Human Metacognitive Control System to Enhance Mental Health. Front. Psychol. 10:2621. doi: 10.3389/fpsyg.2019.02621
- Photo by Tim Foster