
A recent study overviewing the connection between depression and a lack of serotonin in the brain came to the conclusion that there was “…no support for the hypothesis that depression is caused by lowered serotonin activity or concentrations.” (1) Considering that the findings from this study contradict the depression is due to chemical imbalances – theory, how can the causes of depression better be explained?
The metacognitive model of depression explains that rumination, ineffective coping strategies, and the belief that rumination can’t be stopped cause and maintain depression.
There is plenty of evidence that supports the metacognitive model of depression, from studies testing the negative effects of rumination on prolonging depressed mood (2) to how rumination biases thinking and self-judgment (3) and how Metacognitive therapy effectively treats depression when reducing rumination (4)(5).
The metacognitive model of depression explained
- People ruminate, which sustains depressive thoughts and feelings
- Rumination is controlled by metacognitive beliefs that lead people to believe that rumination is a good idea for finding solutions to problems (positive metacognitive beliefs)
- Rumination is also controlled by metacognitive beliefs that rumination is involuntary and uncontrollable (negative metacognitive beliefs)
- Low metacognitive awareness also sustains rumination because people with depression are unaware of how much they ruminate.
- Coping behaviors like withdrawal, excessive sleep, and alcohol backfire and maintain depression.
Professor Adrian Wells, the founder of Metacognitive therapy (MCT), explains that rumination sustains depressive thoughts and feelings. Rumination is driven by metacognitive beliefs that lead people to think that rumination helps solve problems but, at the same time, is also outside of one’s control.
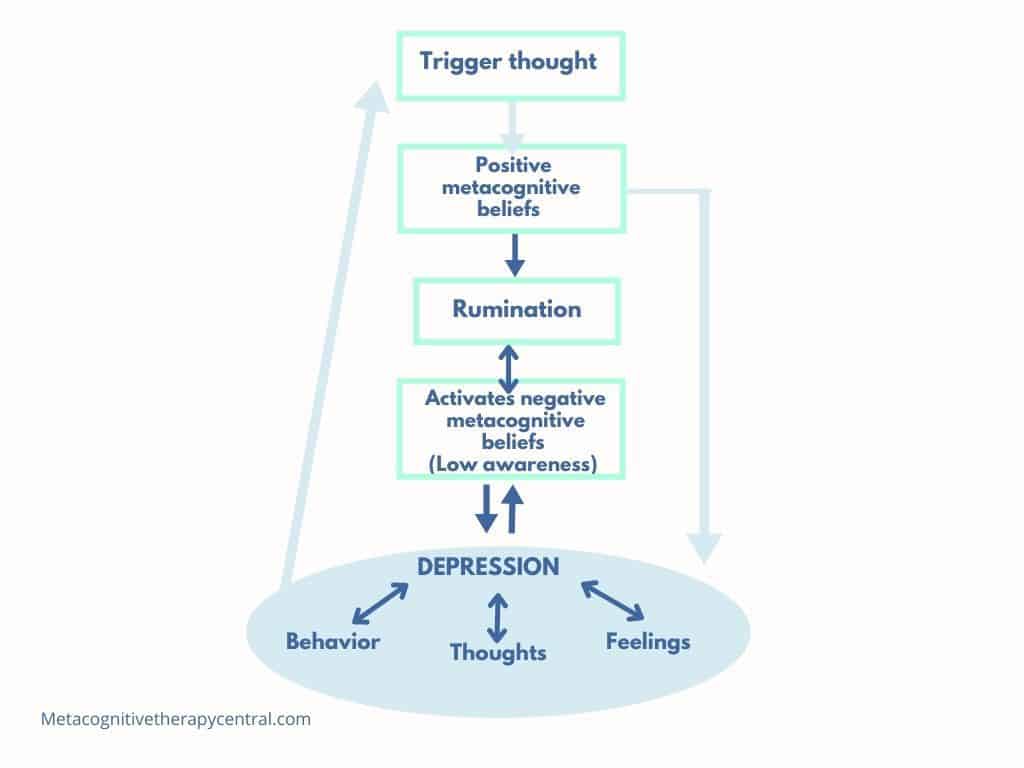
For example, a person is triggered by a negative thought, “I am no good.” If that person believes that he can solve the problem of being no good by ruminating about the thought, he has a metacognitive belief that rumination is helpful. He, therefore, starts ruminating.
However, rumination intensifies and sustains negative emotions like for example, sadness, emptiness, and hopelessness. If this person also believes that he can’t stop ruminating about the thought that he is no good, he has a metacognitive belief that rumination is uncontrollable.
The combination of rumination, intensified negative emotions, and metacognitive beliefs will, according to Metacognitive therapy, cause depression.

How does Metacognitive therapy treat depression?
MCT for depression does not directly focus on reducing the symptoms of depression. Instead, it focuses on teaching the patient that rumination maintains depression. So to recover, the patient has to recognize and reduce ruminations and change her metacognitive beliefs about them (5).
Step 1: Identify the triggers for rumination
A person with depression usually responds to negative thoughts by analyzing them in an attempt to figure out the meaning of events. Examples of triggers for rumination can be:
“Why do I feel this way?”
“What is wrong with me?”
“Will it ever end?”
Rumination is a long chain of thoughts that attempt to figure out the meaning of events (e.g., “Why do I feel this way?”)
Step 2: Notice and reduce rumination
Low awareness is normal in depression and results from worrying and ruminating for a long time. Therefore, many who suffer from depression are unaware of how much time they spend ruminating. Rumination always happens in the background, even when they go about daily activities.
It is therefore important to recognize rumination when it happens and practice reducing it. A helpful way to reduce rumination is through postponement.
Step 3: Eliminate coping behaviors
Coping behaviors in depression include withdrawal, use of alcohol, more rest, and excessive mood checking. But despite their best intentions, coping behaviors backfire because they increase negative thoughts, reduce motivation, and promote rumination.
For example, a person with depression might feel hopeless after many hours of rumination, so he withdraws from daily and social activities to find answers to his hopelessness. Withdrawal, however, only gives more time to rumination without finding solutions.
It is therefore very important to ban coping behaviors and instead increase daily activities.
Using coping strategies to control ruminations only strengthens the belief that rumination can’t be stopped.
Is Metacognitive therapy for depression effective?
Recent studies indicate that MCT significantly reduces depression in around 70% of patients and is more effective than Cognitive-behavioral therapy, CBT.
A large study (7) comparing MCT with CBT for depression found that 74% of the patients who received MCT recovered from depression compared with 52% of the patients who received CBT. The results were unchanged six months after treatment.
Patients who received MCT not only recovered from depression but also improved their metacognitive beliefs, which likely reduces the risk of setbacks.
A recent study comparing depression and anxiety in cardiac rehabilitation (CR) patients showed that when CR patients received MCT, they significantly reduced their depressive and anxious symptoms. Furthermore, they maintained the effect 4 and 12 months after the treatment (8).

Disproving the serotonin theory of depression
The chemical imbalance theory of depression claims that depression is due to serotonin (a chemical produced by nerve cells in the brain) or other chemical abnormalities. This theory has widely influenced the distribution of anti-depressant medication to people suffering from depression.
According to a recent study, however, this understanding of depression leads to a pessimistic outlook on depression, making people depend on medication to regulate their moods (1).
The study did not find convincing evidence that depression is associated with lower serotonin.
Our comprehensive review of the major strands of research on serotonin shows there is no convincing evidence that depression is associated with, or caused by, lower serotonin concentrations or activity.
Moncrieff et. al (2022)
The metacognitive model differs from the chemical imbalance theory by proposing that the brain has an inbuilt ability to self-regulate emotions. So when rumination is reduced, it is possible to recover from depression without the aid of anti-depressant medications (10).
Summary
- The metacognitive model of depression states that depression is caused and maintained by unhelpful coping strategies, mainly rumination.
- Rumination is driven by metacognitive beliefs, which are beliefs about the way we think.
- Ruminations often start with a “Why” sentence and attempt to find solutions to problems.
- Excessive rumination maintains a depressed mood and negatively affects cognitive functions like lower confidence in problem-solving.
References
- Moncrieff, J., Cooper, R.E., Stockmann, T. et al. The serotonin theory of depression: a systematic umbrella review of the evidence. Mol Psychiatry (2022). https://doi.org/10.1038/s41380-022-01661-0
- Nolen-Hoeksema, S. (2000). The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. Journal of Abnormal Psychology, 109(3), 504–511. https://doi.org/10.1037/0021-843X.109.3.504
- Mellings TM, Alden LE. Cognitive processes in social anxiety: the effects of self-focus, rumination and anticipatory processing. Behav Res Ther. 2000 Mar;38(3):243-57. doi: 10.1016/s0005-7967(99)00040-6. PMID: 10665158.
- Solem Stian, Kennair Leif Edward Ottesen, Hagen Roger, Havnen Audun, Nordahl Hans M., Wells Adrian, Hjemdal Odin (2019). Metacognitive Therapy for Depression: A 3-Year Follow-Up Study Assessing Recovery, Relapse, Work Force Participation, and Quality of Life. Frontiers in Psychology 10. https://www.frontiersin.org/articles/10.3389/fpsyg.2019.02908
- Wells A (2008). Metacognitive Therapy for Anxiety and Depression: New York: Guilford Press
- Photo by Christopher Lemercier – Unsplash
- Callesen, P., Reeves, D., Heal, C. et al. Metacognitive Therapy versus Cognitive Behaviour Therapy in Adults with Major Depression: A Parallel Single-Blind Randomised Trial. Sci Rep 10, 7878 (2020). https://doi.org/10.1038/s41598-020-64577-1
- Wells et. al, Circulation Volume 144, Issue 1, 6 July 2021 https://doi.org/10.1161/CIRCULATIONAHA.120.052428
- Photo by Kulli Kittus – Unsplash
- Wells, Adrian & Matthews, Gerald. (1996). Modelling cognition in emotional disorder: The S-REF model. Behaviour Research and Therapy. 34. 881-888. 10.1016/S0005-7967(96)00050-2.
- Photo by Malicki M. Beser – Unsplash



