
Frantic efforts to avoid real or imagined abandonment, unstable relationships, intense mood swings, and self-harming behaviors are some of the features that make Borderline personality disorder difficult to treat.
According to MCT, BPD symptoms can be seen as unhelpful coping strategies that patients with BPD use to manage intense feelings like anxiety, sadness, emptiness, and shame. However, these feelings can be managed through strategies like detached mindfulness.
Learning to control intense feelings through detached mindfulness will help BPD patients eliminate these unhelpful coping behaviors and achieve partial or full recovery from BPD.
People who suffer from BPD use unhelpful coping strategies like self-harm, substance abuse, worry, and rumination to manage intense feelings like anxiety, sadness, emptiness, anger, and shame.
Why is MCT an effective treatment for Borderline personality disorder?
Metacognitive therapy is effective for BPD because
- MCT helps patients with BPD tolerate more distress and disengage from it
- MCT helps give BPD patients a greater sense of stability and less engagement in suicidal behaviors
- MCT teaches BPD patients to achieve cognitive flexibility (to have many choices of responses to distressing thoughts and feelings)
- MCT helps create a sense of personal responsibility for own actions
- MCT helps BPD patients develop a capacity for stable relationships with friends and partners
What is Borderline personality disorder?
Borderline Personality Disorder (BPD) is characterized by a chronic, prevalent pattern of instability in interpersonal relationships and dysregulated emotions. People who suffer from BPD desperately attempt to avoid real or imagined abandonment, have very intense relationships, have difficulty controlling anger, and engage in self-harming behaviors (2) (3).
| DSM-V Borderline personality disorder diagnosis criteria | Symptom category |
| Frantic effort to avoid real or imagined abandonment | Affective |
| Identity disturbance | Affective |
| Reactivity of mood | Affective |
| Chronic feeling of emptiness | Affective |
| Stress-related paranoid ideation | Affective |
| Unstable intense interpersonal relationships, switching between idealization and devaluations | Interpersonal |
| Difficulty controlling anger, they become agitated and aggressive | Interpersonal |
| Self-harming and suicide attempts | Impulse control |
| Impulsivity | Impulse control |
Patients with BPD have the following problems in common:
- Severe problems in dealing with themselves, their mind, behavior
- Executive problems (lack of concentration, poor memory)
- History of impulsivity
- Misuse substances (dealing with difficulties by self-harming)
These problems have the following consequences (3):
1) Functional impairment
BPD is very functionally impairing, which shows through the many BPD patients attending outpatient (10%) and inpatient (20%) treatment clinics and hospitals.
These high rates are partly because people with BPD engage in suicidal behaviors and deliberate self-harm. Unfortunately, some of these patients commit suicide, often because some of their self-harming behaviors get out of control.
2) Chronic course of illness
Most of these patients receive six years of therapy on average. Their reason for attending therapy is when they are distressed by interpersonal conflict with their partner, friends, or parents.
Many drop out of therapy or skip sessions too early, and when their distressing situation changes for the better. However, this pattern of attending and suddenly dropping out of therapy contributes to a bad recovery prognosis.
75% of BPD patients attempt suicide at one point in their lives, and those who engage in self-harm may experience further functional impairment.
3) Co-occurring psychiatric disorders
BPD patients usually suffer from other psychiatric disorders like anxiety (21-59%) and depression (29-50%). This doesn’t only impact the BPD patients but also their interpersonal relationships, creating troubled and unstable relationships.
4) Interpersonal instability
People with BPD engage in more hostile interpersonal communications in their romantic and other relationships than those without BPD.
Usually, they are triggered by rejection or signs of abandonment (“What if she leaves me?“) and have feelings of anxiety, anger, and despair that they don’t know how to deal with. Therefore, they end up worrying and self-harming, which only exacerbates their distress, leading to more interpersonal conflict.

Is it possible to recover from BPD?
Research (5) suggests that the prognosis (the recovery rate) for most BPD patients is better than previously recognized. The majority of patients with BPD experience substantial reductions in their symptoms much sooner than previously known.
The current recommended treatment for BPD is Dialectical Behavior Therapy (DBT), which includes acceptance (non-judgemental attitude, attention to the present moment) combined with promoting healthy change in interpersonal interactions (analyzing unhelpful behaviors and learning problem-solving skills) (6).
38-58% of patients with borderline personality disorder recover through treatment with DBT; however, 48% relapse after 2 years. DBT treatment is often long-term (between 24.36 months) and resource-demanding.
A large study of 202 BPD patients shows the following:
Although the remission rates look much better than assumed (75% of BPD patients recover after six years), BPD patients don’t recover much from mood swings, low or anxious moods, and anger (also called affective symptoms).
Psychologists assume that the lack of improvement in affective symptoms is part of people with BPD’s identity and temperament and, therefore, resistant to change.
Metacognitive therapy offers a different perspective on the lack of improvement in affective symptoms. According to MCT, the lack of improvement from mood swings, anxiety, and low mood is due to prolonged worry and rumination.

How Metacognitive therapy treats BPD
According to MCT, borderline personality disorder is maintained through unhelpful coping strategies like rumination, worry, self-harm, and the belief that feelings are dangerous and can’t be controlled.
Metacognitive therapy (MCT) does not view BPD as a biological disease that is difficult to treat. Instead, BPD is maintained by the many unhelpful coping strategies that patients with BPD use to manage their intense feelings.
According to Metacognitive therapy, people with BPD believe that intense feelings can make them lose control or go crazy. Therefore they ruminate, worry, and self-harm to try to cope with their feelings. However, these strategies backfire and create more intense feelings.
- I will lose it if I get too stressed
- I have no control of my mind
- If I feel rejected/abandoned, I will go mad
- Feelings can destroy me
- Too much thinking and negative thoughts can drive me crazy
- Negative thinking can make me do bad things
When someone with BPD believes that intense feelings are uncontrollable and dangerous, they will go to great lengths to cope with their negative feelings. This is done by activating unhelpful coping behaviors, also called the cognitive attentional syndrome (CAS).
CAS in BPD
self-harm
Avoidance
Substance abuse
Risk-taking
thought-suppression
rumination
paranoid thinking
Acting out
suicidal thinking
worry
Often, patients with BPD also have the following beliefs about their thinking:
- If I worry, I will be more in control
- Rumination helps me sort my mind
- I need to feel better before I can move on with my life
- I need to feel in control before I can move on with life
As shown here, patients with BPD have many metacognitive beliefs that have negative and self-defeating characteristics. Encountering BPD patients with these beliefs can seem incredibly overwhelming in therapy, and if left unaddressed, induce hopelessness for both the therapist and the patient.
Metacognitive therapy views these limiting beliefs as voluntary coping strategies that BPD patients deliberately use to cope with their thoughts and intense feelings. BPD patients use these strategies to gain control when experiencing rejection and pain (pain=anxiety) (3).
Viewing these beliefs as voluntary coping strategies (instead of symptoms) makes it possible to learn to stop doing them. Unfortunately, BPD patients sometimes lack awareness of how they use these strategies to deal with their distress. More importantly, they miss the fact that these very strategies maintain their disorder.
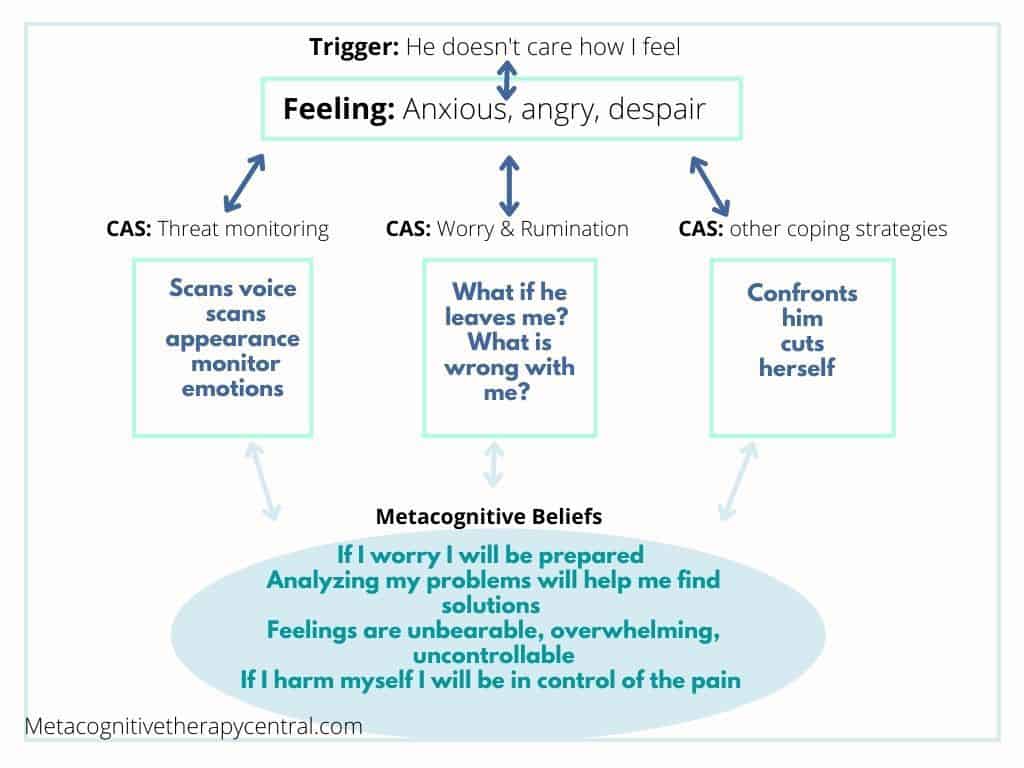
When patients with BPD are distressed, they believe that something bad or dangerous can happen because they generally believe that feelings are overwhelming, unbearable, and uncontrollable. Usually, they are triggered by rejection or signs of abandonment (“What if he leaves me?“) and have feelings of anxiety, anger, and despair.
They then try to cope with these feelings through worry, rumination, threat-monitoring, and self-harm. However, these strategies backfire because they block healthy emotional processing, leaving the person with BPD in a negative spiral of intense feelings and unhelpful coping strategies.
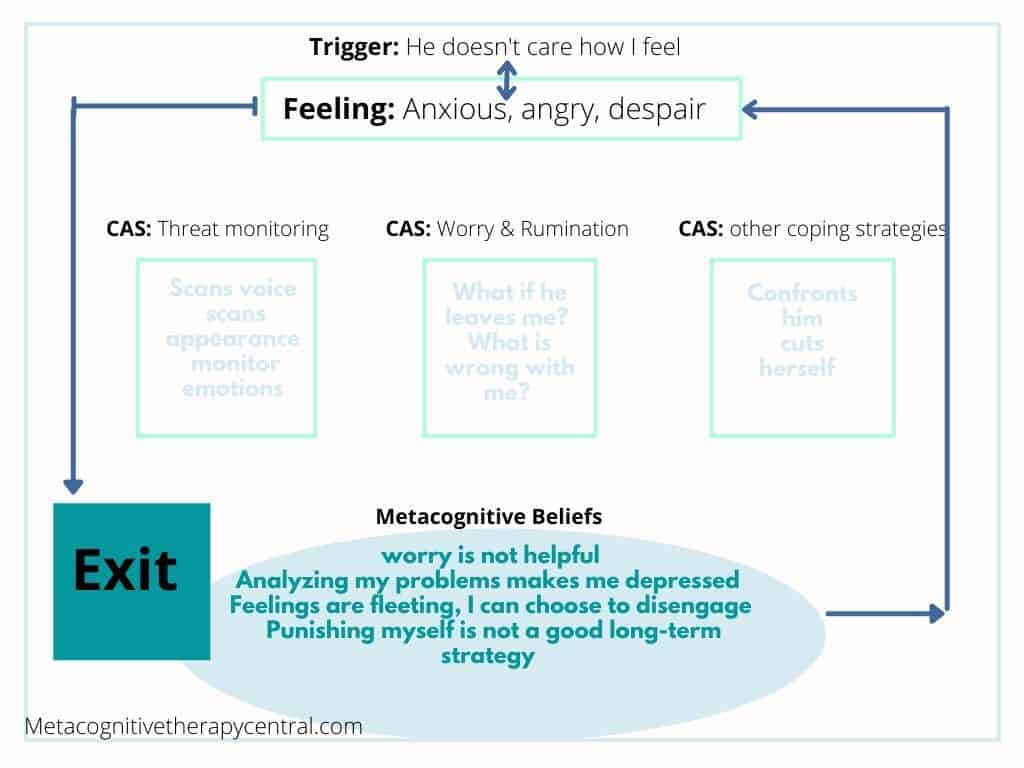
In order to stop the negative spiral, their negative metacognitive beliefs need to be challenged and changed:
| From believing: | To believing |
| If I worry, I am prepared | Worry is not helpful |
| Rumination will help me find answers | Rumination is not the best way to solve problems |
| If I punish myself, I am in control of the pain | Punishing myself is not a long-term strategy |
Reducing worry/rumination means engaging less in self-harming behaviors (as these are used in an effort to stop intense feelings) and thereby achieving healthy emotional processing. And the only way to reduce worry/rumination/self-harming behaviors is to change false (metacognitive beliefs) about these strategies being helpful. This can be achieved through Metacognitive therapy.
The most important reason behind MCT’s success in treating BPD is viewing BPD symptoms as voluntary strategies that maintain BPD.
Voluntary unhelpful coping strategies can be reduced and stopped, compared with symptoms that are involuntary side effects.
| These features are usually seen in other therapies as involuntary symptoms | How MCT sees them as voluntary strategies |
| Suicidal thinking | Ruminating about committing suicide |
| Paranoid thinking | Ruminating about paranoid thoughts |
| Thought suppression | Trying not to think about distressing thoughts/events |
| Dissociation | Internally focused attention and rumination |
| Risk-taking | Following an urge/feeling/thought |
| Substance abuse | Using alcohol/drugs to numb distressing feelings |
| Avoidance | Staying away from people/uncomfortable situations Avoid doing chores |
| Self-harm | Behavior used to control distressing feelings / numb out intense feelings |
| Fighting/acting out | Following an urge/feeling Trying to find relief from distressing feelings |
For example, current models of BPD view self-harming, avoidance, and fighting/acting out as involuntary symptoms people with BPD have. MCT views these symptoms as strategies that people with BPD use to calm their intense feelings and negative thoughts when they are triggered. Since these strategies maintain BPD, MCT teaches new ways of dealing with intense feelings instead (3) (9).
MCT reduces rumination in BPD
Rumination is often very prominent in patients with BPD. They are super-ruminators and engage in angry, self-pity, and shame ruminations:
Examples of ruminations – depressive (self-pity and shame): “Why am I abnormal? Why am I unlovable? Why do I feel like this?“
Examples of angry ruminations: “Why am I not treated fairly? Why is it always me to blame? Why am I always the scapegoat!”
When someone with BPD becomes upset in response to a triggering event (for example, when feeling rejected by someone) or experiences a negative mood, they begin to ruminate, which maintains and exacerbates their negative mood.
For example, a person with BPD gets into a heated argument with a close friend and becomes upset. She begins to dwell on the argument, how her friend hurt her, and how badly she is currently feeling. In turn, this ruminative process will prolong her distress and make her ruminate even more.
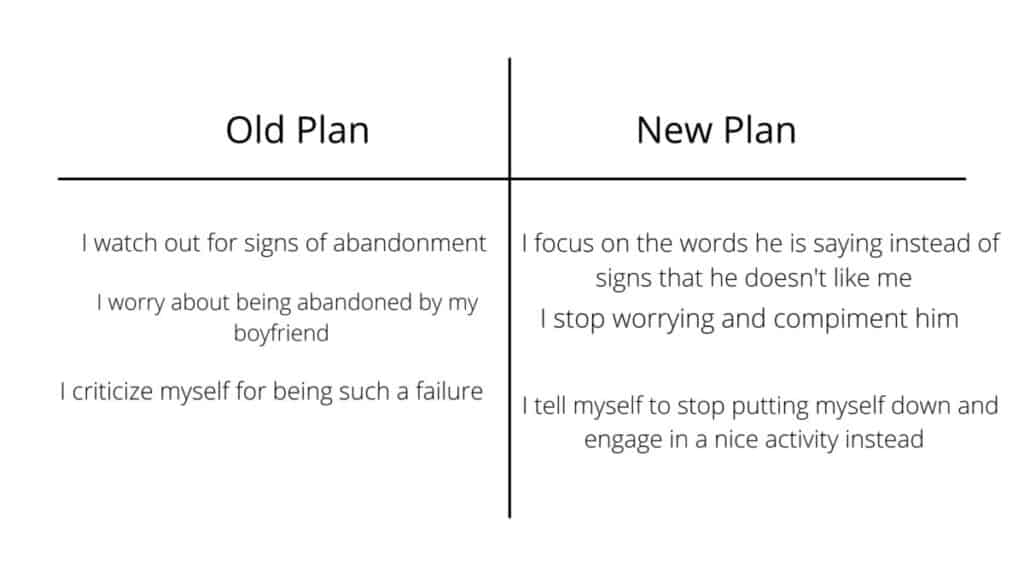
In Metacognitive therapy, BPD patients learn to identify and reduce rumination. So instead of ruminating about how badly she was treated, the BPD patient learns to identify what she is doing (ruminating herself into sadness and depression) and postpone ruminating till later.
Postponing rumination (and worry) prevents prolonged negative mood and helps the patient distance herself from her negative thoughts and feelings. This will helps her process emotions in healthier ways, making them dissolve on their own.

MCT reduces interpersonal problems
People with BPD are usually triggered by interpersonal conflict and perceived signs of rejection. This makes them activate rumination as a problem-solving strategy, and if that fails, they self-harm or continue to create more conflict.
If I face rejection – I will lose it, go insane
My feelings are overwhelming and can destroy me
The literature shows that people with BPD have a heightened sensitivity to interpersonal settings. For example, patients with BPD over-evaluate others’ emotional states and intentions, a known risk factor for interpersonal conflict and distress (10).
Besides, interpersonal triggers lead to more intense feelings, and patients with BPD experience more disagreement and ambivalence in social situations than people without BPD. As a coping response, people with BPD start ruminating and worrying when experiencing social difficulties.
“Watching signs of abandonment will make me alert and ready for it”
The aim of MCT is to challenge these false metacognitive beliefs so that the BPD patient learns that feelings don’t have such power and, in fact, are very fleeting. Once BPD patients change their relationship with intense feelings like abandonment and rejection, they are more willing to disengage from them instead of stirring up more conflict in their relationships.
Research on MCT for BPD
Research shows that BPD patients achieve large improvements over time with MCT. Mainly, borderline symptoms severity, interpersonal problems, and trauma symptoms improve, and these treatment gains are maintained two years after (8).
Summary
- BPD is maintained by the CAS and limiting beliefs about feelings and thinking
- The CAS for BPD consists of worry, rumination, and self-defeating behaviors (among others)
- MCT can teach patients with BPD to reduce rumination and worry and cope with anxiety, anger, sadness, and shame in healthier ways
- Research shows that reducing the CAS will help reduce BPD symptoms and this effect is still maintained after two years
If you are suffering from BPD, it is important that you seek out an MCT-I-certified therapist. An MCT-I certified therapist will make sure to follow a research-based approach that guarantees quality treatment and help you with a faster recovery.
References
- Photo by Hannah Xu
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
- Hans Nordahl, personal communication, Copenhagen 2021
- Photo by Claudia Wolff
- Zanarini MC, Frankenburg FR, Hennen J, Silk KR. The longitudinal course of borderline psychopathology: 6-year prospective follow-up of the phenomenology of borderline personality disorder. Am J Psychiatry. 2003 Feb;160(2):274-83. doi: 10.1176/appi.ajp.160.2.274. PMID: 12562573.
- Dimeff, L., & Linehan, M. M. (2001). Dialectical behavior therapy in a nutshell. The California Psychologist, 34(3), 10-13.
- Photo by Christina-wocintechchat
- Nordahl HM and Wells A (2019) Metacognitive Therapy of Early Traumatized Patients With Borderline Personality Disorder: A Phase-II Baseline Controlled Trial. Front. Psychol. 10:1694 doi: 10.3389/fpsyg.2019.01694
- Gratz KL, Roemer L. The relationship between emotion dysregulation and deliberate self-harm among female undergraduate students at an urban commuter university. Cogn Behav Ther. 2008;37(1):14-25. doi: 10.1080/16506070701819524. PMID: 18365795.
- Glenn, Catherine & Klonsky, E David. (2009). Emotion Dysregulation as a Core Feature of Borderline Personality Disorder. Journal of personality disorders. 23. 20-8. 10.1521/pedi.2009.23.1.20.



